It evolves severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) transmission and subsequent airway inflammation due to viral infection.
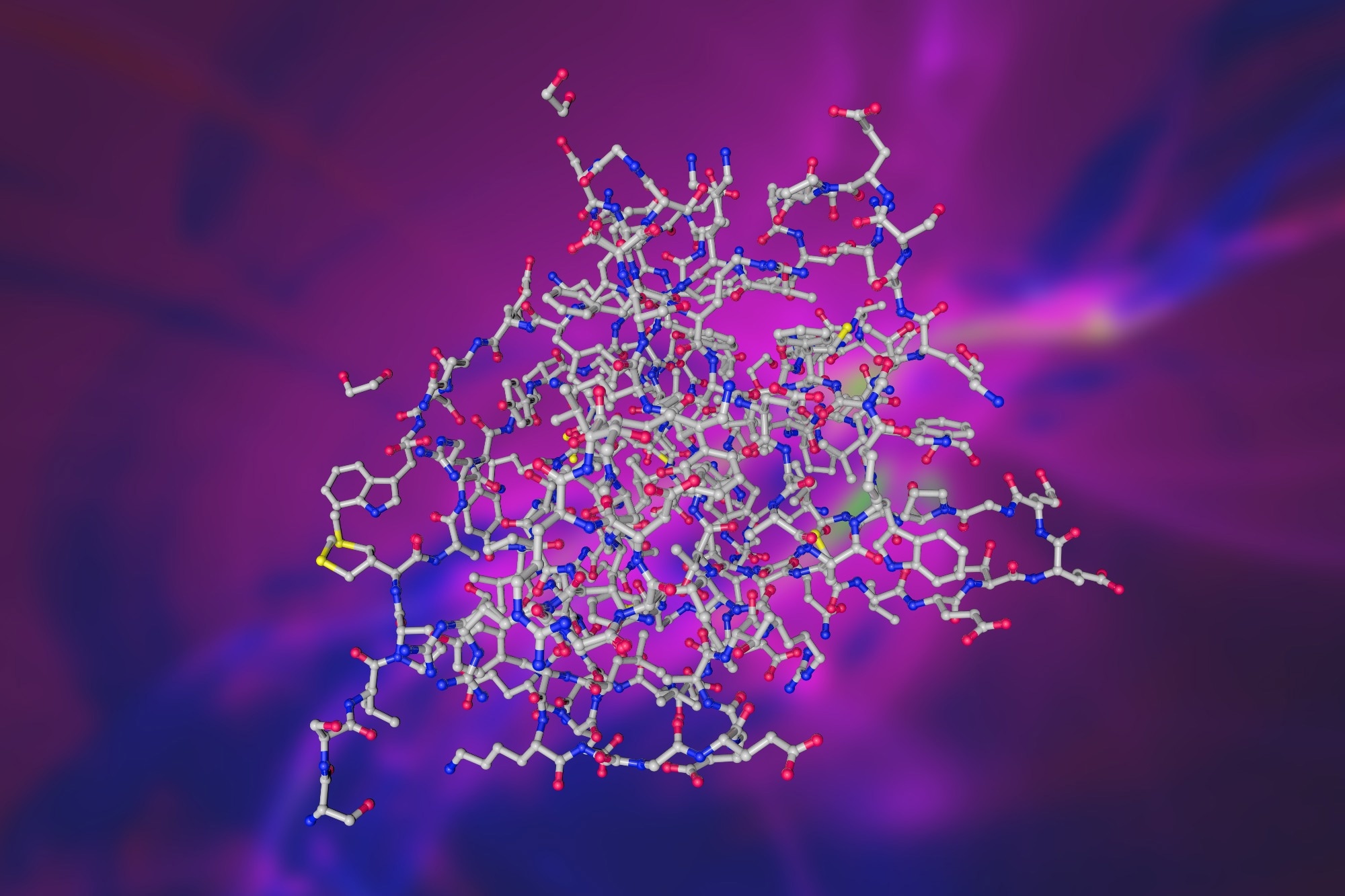 Study: IL-9 aggravates SARS-CoV-2 infection and exacerbates associated airway inflammation. Image Credit: MarynaOlyak/Shutterstock.com
Study: IL-9 aggravates SARS-CoV-2 infection and exacerbates associated airway inflammation. Image Credit: MarynaOlyak/Shutterstock.com
Background
SARS-CoV-2 infection could induce acute respiratory distress syndrome (ARDS), a lethal condition arising from immune cells' hyperactivation that triggers bronchoalveolar inflammation, inflammatory cascade, and COVID-19-related immunopathology.
Thus, anti-inflammatory drugs, like dexamethasone, could lower the severity of COVID-19-induced respiratory symptoms and lower mortality. In general, immune suppression is an effective COVID-19 mitigation tool, at least against pulmonary pathologies of COVID-19.
Il-9 is a gamma (γ) chain family cytokine mainly produced by Th9 cells, a subpopulation of CD4+T cells. A key transcription factor, Pu.1 is essential for IL-9 induction and Th9 cell differentiation. Forkhead Box Protein O1 (Foxo1) is another essential transcription factor for IL-9 induction in Th cells.
IL-9 promotes mast cell growth and plays a role in allergic inflammation. Likewise, its role in severe airway inflammation and bronchial hyperresponsiveness caused by Respiratory Syncytial Virus (RSV) infection and asthma is well-recognized.
However, scientists have not yet uncovered the role of IL-9 in SARS-CoV-2-associated immunopathology.
About the study
The present study used six- to eight-week-old male and female hACE2.Tg mice to administer live SARS-CoV-2 and perform all the study experiments. They cohoused infected mice with the uninfected ACE2.Tg mice in a 1:1 ratio 24 hours post-infection (pi) to monitor mice for COVID-19 symptoms and measure their other parameters.
The researchers used lung tissue and fecal samples of all test animals for measuring viral load, i.e., the relative copy number of SARS-CoV-2 ribonucleic acid (RNA) and their relative gene expression.
While they used Foxo1fl/fl mice to study the role of IL-9, bronchoalveolar lavage fluid (BALF) from test animals' lungs helped them quantify IL-4/9/10 and interferon-gamma (IFN-γ) by enzyme-linked immunosorbent assay (ELISA).
Further, the team used peripheral mononuclear blood cells (PBMCs) from healthy human donors to isolate RNA and test the expression of respective genes relative to β-Actin by reverse transcription-polymerase chain reaction (RT-PCR).
The team further normalized the relative gene expression levels by log2 transformation to calculate Z-scores. Eventually, they represented the median of Z-scores of log2 transformed relative gene expression as a heat map.
In a substudy, the team randomly selected five mice to assess the comparative therapeutic effects of vehicle, remdesivir (RDV), or Foxo1 inhibitors. In another substudy, they examined the therapeutic effects of suboptimal (S.O.) αIL-9 and RDV when administered once daily via intraperitoneal injection.
Results
So far, studies have not deciphered whether adaptive immune cells, particularly CD4+ and CD8+ T cells, regulate anti-SARS-CoV-2 response and airway inflammation though they confer protection against primary SARS-CoV-2 infection.
In this study, the researchers demonstrated that the Foxo1-IL-9 axis controlled two distinct pathological features of COVID-19 - viz., anti-viral pathway and airway inflammation.
Accordingly, they noted that IL-9 was upregulated in SARS-CoV2-infected-ACE2.Tg mice, whereas its depletion enhanced viral clearance by regulating SARS-CoV-2-induced airway inflammation and lung pathology.
Previous studies have also established that IL-9 triggers mast cell hyperplasia and mucus production. Thus, anti-IL-9 neutralization decreases allergic inflammation.
In agreement with these findings, current study results showed that ceasing IL-9 neutralization in SARS-CoV-2-infected animals could help reduce histopathological scores and decrease collagen deposition, mucus production, and mast cell accumulation in the lungs of all test animals.
Together, this data indicated that IL-9 and mast cells crosstalk during SARS-CoV-2 infection, consistent with the prior findings that IL-9 favors mastocytosis.
Further, the study data demonstrated that Foxo1 deficiency in CD4+ T cells blunted IL-9 production, which made test animals less vulnerable to SARS-CoV-2 infection and virus-induced airway inflammation.
Intriguingly, exogenous IL-9 transfer in Foxo1-sufficient CD4+ T cells made Foxo1-deficient mice susceptible to SARS-CoV-2 infection, further confirming that Foxo1-Il-9 mediated Th cell-specific pathway played a role in COVID-19 pathogenesis.
Conclusions
Collectively, the current study provided much-needed mechanistic insights into important proinflammatory pathways involved in SARS-CoV-2 infection and presented proof of principle that host-directed therapeutics against IL-9 could help mitigate COVID-19 severity, especially pulmonary complications arising due to SARS-CoV-2 infection.