A comprehensive review of food allergy (FA)-related studies published between 2021 and 2023 is currently in press with the Journal of Allergy and Clinical Immunology. This article highlights the increasing burden of FA in the developing world, gradual stabilization in Europe and other developed regions, and promising research into the mechanisms that cause FA and its diagnosis and treatment.
Environmental factors, genetics, and prevalence of FA
The incidence of FA has historically been more common in urban areas and developed nations, with one estimate suggesting that the pooled lifetime prevalence is as high as 19.9% in Europe. Nonspecific lipid transfer proteins (nSLTP) are the most common cause of FA in Southern Europe and are becoming more widespread across the rest of Europe, Latin America, China, and Japan.
Environmental changes and ethnicity may have a joint role in the development of FA, as indicated by an estimated FA prevalence of 15% among Australian children with Asian heritage compared with 1.1% for those with Singaporean heritage. Studies on the role of genetics have identified human leukocyte antigens (HLAs) that are associated with certain FAs, such as single nucleotide polymorphism (SNP) rs9277630 and HLA-DPB1*02:01:02 for wheat allergies.
Hospital admissions for FA-related anaphylaxis have risen sharply over time, with this reaction disproportionately affecting teenage and younger children. While the number of fatalities has remained stable, nuts and cow milk allergies are the leading cause of death from FA-induced anaphylaxis.
Mouse and human in-vitro studies examine FA mechanisms
A mouse study found that individuals who were given peanut butter while also exposed to peanuts in their environment were less likely to become sensitive and allergic, which could be mediated by cytotoxic T-lymphocyte-associated protein 4 (CTLA-4) and induction of T-regulatory cells. Other studies indicated that damage to the gut epithelial barrier (such as by dishwater detergents) could cause FA.
Loss-of-function mutations within the filaggrin gene are now thought to be associated with the persistence of egg and cow’s milk allergies. Alpha-gal, which is present in glycolipids and glycoproteins, may contribute to peanut allergies. However, Ara h 2 is the dominant peanut allergen and may form complexes with Ara h 1 and Ara h 3, leading to cross-reactivity and a biased estimation of the immunological importance of the latter two.
An interesting study on peanut-allergic patients found distinct biomarkers in patients with lower thresholds of peanut tolerance, such as higher peanut-specific immunoglobulin E (IgE) levels and peanut-specific IgE/IgG4 ratios. A lower reactivity threshold was associated with the presence of peanut-specific Th2 cells, which were successfully eliminated by oral immunotherapy. Other studies showed that clinical phenotypes interact with allergen-specific IgE traits, which are then reflected in basophil responses.
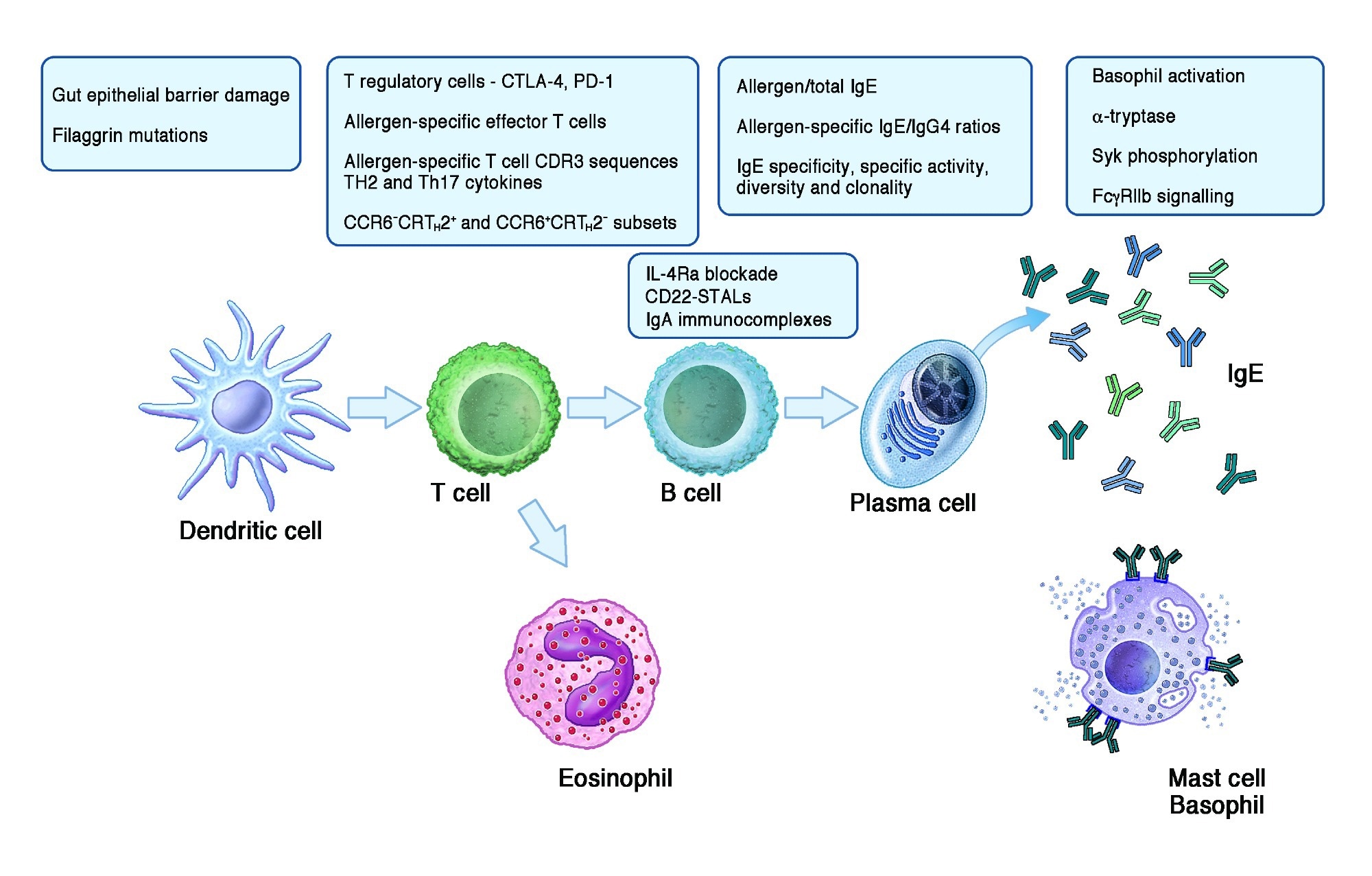 Highlights on the topics of the novel publications about mechanisms of food allergy and tolerance mentioned in the text. Figure built with Biorender.
Highlights on the topics of the novel publications about mechanisms of food allergy and tolerance mentioned in the text. Figure built with Biorender.
Developments in FA diagnosis and clinical guidelines
The gold standard for the definitive diagnosis of FA is considered to be the oral food challenge (OFC), which is expensive, time-consuming, and can lead to severe allergic reactions. However, guidelines with less rigid challenge stop criteria and more subjective symptoms could lead to the overestimation of FA without reducing rates of anaphylaxis.
Recent systematic reviews and meta-analyses have highlighted functional specificity and sensitivity cut-offs to guide allergy test result interpretation. Extensive population-based longitudinal studies are required to better understand risk factors for FA severity, but new scoring systems such as the Food Allergy Severity Score (FASS) and the Definition of Food Allergy Severity (DEFASE) are important developments.
The basophil activation test (BAT) is a promising new test that has been integrated into clinical practice. The BAT is a flow cytometry-based test involving all components of the reaction, including serum IgE (sIgE), effector cells, and other antibodies. It has emerged as the best predictor of allergic reaction thresholds and severity to baked eggs in terms of accuracy, specificity, and sensitivity while also demonstrating high reliability and reproducibility across multiple laboratories. While other tests, such as peptide-specific IgE, also have potential, they require further validation and research.
New therapies, drugs, and vaccines
Ongoing research highlights the role of newer therapies, medicines, and vaccines in tackling FA. For example, oral immunotherapy (OIT) has been shown to increase desensitization, sustained unresponsiveness, and even consumption of milk and peanuts for preschool-aged children. However, further research is needed to determine its long-term effects.
Similarly, epicutaneous immunotherapy (EPIT) has been established as well-tolerated and safe for children with peanut allergies but has also not been studied in the long term. Sublingual immunotherapy (SLIT) is being tested in combination with OIT to treat cow’s milk allergies, while oral mucosal immunotherapy (OMIT) may allow the delivery of higher doses of allergens.
Among drugs being tested to reduce the severity of allergies, omalizumab appears to reduce reactions and improve the quality of life for people with allergies while also increasing the dose of allergens they can tolerate. Higher doses of omalizumab are more effective without an associated increase in adverse effects.
Other medications currently being tested include ligelizumab, abrocitinib, abatacept, and remibrutinib. Since gut microbial diversity, composition, and metabolic activity are associated with food tolerance and allergy, probiotics are also being studied for FA relief and appear to be more beneficial for cow’s milk allergies than peanut allergies. Fusion and mRNA vaccines are also in development.
Emerging evidence: Is it possible to prevent food allergies?
Studies have explored the links between dietary diversity during pregnancy and the first year of life, with results indicating that yogurt and vegetables reduce the incidence of allergic disease but not FA.
An ongoing trial focuses on whether consuming allergenic food items during pregnancy could reduce the offspring’s risk of developing FA. At the same time, another study is investigating whether probiotics could reduce egg, wheat, soya, and cow’s milk allergy-related symptoms in month-old infants.
Skin interventions such as emollients have been evaluated, with concerning findings that they can increase FA risk and not prevent it. The early introduction of peanuts to infant diets has not been shown to reduce peanut allergy prevalence, based on a trial in Australia.
Conclusions
Overall, this comprehensive analysis of recent advances in FA-related research highlights the importance of emerging studies in improving the diagnosis and management of various allergies and indicates avenues for further investigation. The results of ongoing trials are eagerly awaited by the medical community and individuals living with food allergies and their families.