Feb 28 2005
Results of a new study suggest that the higher prevalence of celiac disease in individuals with osteoporosis than in the general population may justify screening of patients with osteoporosis for celiac disease, according to an article in the February 28 issue of Archives of Internal Medicine, one of the JAMA/Archives journals.
Patients with celiac disease have an inappropriate immune response to gluten, a component of wheat proteins, which makes it difficult to properly digest many foods, according to background information in the article. Although adults diagnosed with celiac disease commonly have a low bone mineral density (BMD) and treatment with a gluten-free diet increases their BMD, there has not been clear evidence of the benefit of screening everyone with osteoporosis for celiac disease.
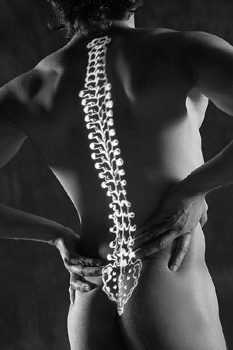
Osteoporosis is the loss of bony tissue, resulting in bones that become brittle and liable to fracture. Infection, injury and synovitis (inflammation of the membrane surrounding a joint), as well as prolonged exposure to microgravity, can cause osteoporosis.
William F. Stenson, M.D., of Washington University School of Medicine, St. Louis, and colleagues evaluated 840 individuals, 266 with and 574 without osteoporosis from the Washington University Bone Clinic by serologic screening for celiac disease (blood test for antibodies associated with celiac disease). The diagnosis of celiac disease was then confirmed with an intestinal biopsy and individuals with a confirmed diagnosis were treated with a gluten-free diet and followed up for improvement in BMD.
Twelve of the 266 patients with osteoporosis and six of those without osteoporosis tested positive by serological screening for celiac disease, the researchers found. Nine patients with osteoporosis (3.4 percent) and one of those without osteoporosis (0.2 percent) had biopsy-proven celiac disease. Further, the authors write, ".the more severe the celiac disease, the more severe the resulting osteoporosis."
"Treatment with a gluten-free diet for a year resulted in improved BMD in individuals with celiac disease and osteoporosis," the authors write. "The improvement in BMD for celiac disease patients on the gluten-free diet was greater than that expected for osteoporotic patients receiving standard therapy."
"In conclusion, we found that the prevalence of celiac disease among osteoporotic patients was much higher than among the nonosteoporotic population and high enough to justify a recommendation that all individuals with osteoporosis undergo serologic screening for celiac disease," the researchers state. ".individuals with positive serological screening should be evaluated with endoscopy and small-intestine mucosal biopsy to establish the diagnosis of celiac disease. Treatment of these individuals with a gluten-free diet will improve their BMD."