The poorest and most socially deprived areas in England have the highest rates of prescription for benzodiazepines and Z-drugs, according to a new University of Warwick study published in the journal Family Practice on October 22, 2019. These pills are strong sedatives and are also prescribed to reduce anxiety. Due to their strong addiction potential, in most cases they are meant to be used for only short periods, to stabilize patients until they are able to cope with anxiety on their own or to get better sleep.
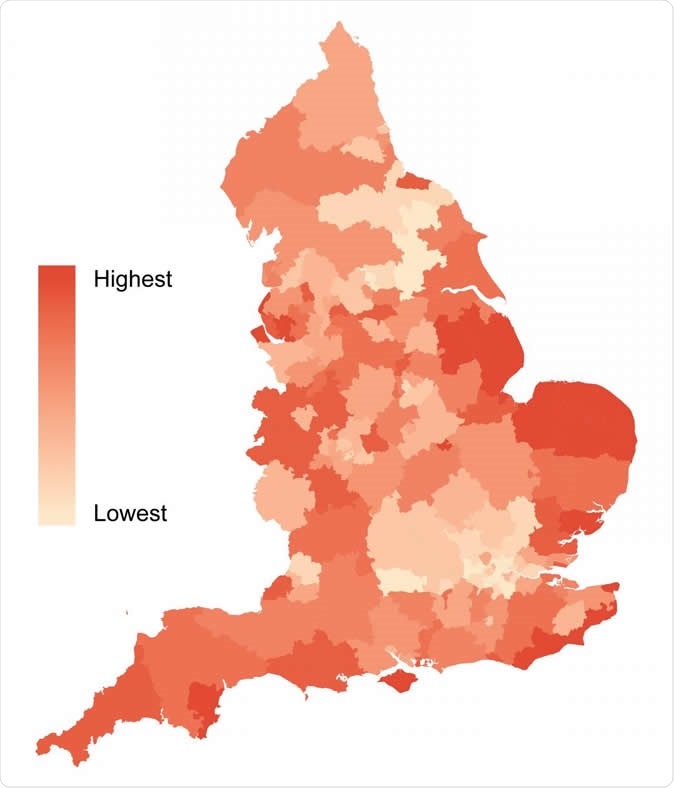
Geographical variation in the prescribing rate of benzodiazepines and Z-drugs across England in 2017 by Clinical Commissioning Group. Image Credit: University of Warwick
Benzodiazepines and Z-drugs
There were more than 14 million prescriptions for these drugs in 2017, which is equivalent to over 2 billion mg of diazepam. About 300 000 patients in the UK are taking long-term prescriptions for benzodiazepines which, along with Z-drugs like zopiclone, are drugs used to treat insomnia and other sleep problems, anxiety, and alcohol withdrawal symptoms. Most of the recipients are elderly people. However, when prescribed for the control of anxiety or painful conditions, the patients may be of any age. In fact, some younger patients are prescribed a benzodiazepine for acute back pain.
The issue with benzodiazepines is their tendency to induce dependency and addiction after they have been used for a long time. Their use is also linked to side effects, such as a higher risk of falls, a loss of ability to drive leading to an increased rate of accidents, a tendency to overdose by accident, reduced cognitive ability and dementia, especially when used by older people – for whom they are mostly prescribed.
The study
The study examined the rate at which Z-drugs were prescribed in a wide variety of GP practices in 2017, throughout England in order to find out for whom these prescriptions were being issued. This was then compared with the degree of social and economic progress in each of the locations examined.
The researchers drew prescribing information from the NHS Digital database of GP practice, and also used the Index of Multiple Deprivation scores derived for each practice’s geographical area by Public Health England. They also examined the demographic characteristics for each practice area, using data from NHS Digital.
The Index of Multiple Deprivation scores are comprehensive measures of deprivation for the population of a particular area. These are calculated on the basis of deprivation in seven fields, namely:
- Income
- Employment
- Health deprivation and disability
- Education
- Skills and training
- Housing and services
- Living environment deprivation, and crime
The findings
The study showed that the volume of benzodiazepines prescription is closely linked to social and economic deprivation, even after adjusting for the effects of age and sex differences in the treated populations within the practice areas of different GPs. The rate of prescription was about 45% higher in the most deprived area of GP practice compared to the least deprived. In terms of the number of prescriptions, there were 288 prescriptions per 1000 patients vs 198 per 1000 in the most and least deprived populations respectively.
High prescription rates are also found in coastal areas of England, but there is considerable variation between prescription rates in different population characteristics in these regions. For instance, religious cultures may lead to relatively low levels of alcohol abuse, which in turn may lead to a lower need for drugs like chlordiazepoxide which are often used to help with quitting alcoholics.
Commenting on the observed connection between the number of prescriptions for these drugs and the level of socioeconomic deprivation of the people in that area, researcher Saran Shantikumar says that they still can’t find out which people are getting the prescriptions within each practice. He cites a recent Public Health England study that says that on an individual basis, patients from the most privileged areas are the most likely to get these prescription – which would mean that fewer individual patients are being given these drugs in the most deprived areas. If so, the puzzle is how fewer patients are receiving a higher amount of these drugs.
He goes on to speculate, “One possibility is that the reasons for prescribing are systematically different between practices with high or low deprivation, and that those in more deprived practices are more likely to be given repeat prescriptions.” This is more likely to be the case, given that different benzodiazepines are related in different ways to deprivation and prescription patterns. Moreover, the Index of Multiple Deprivation scores are not individually determined for those patients on the drugs, and therefore there is no certainty that deprived patients have higher odds of being prescribed benzodiazepines or Z-drugs. Thus more work is necessary to find drug-specific associations.
The implications
The high volume of benzodiazepine prescribing in deprived areas should wake physicians up to the fact that some of their patients may have been on these drugs over the long term, increasing their medical and addiction risk. As the researchers note, Public Health England has recently reported that these drugs are being taken by a lot of people, and some for a very long time. All doctors who have faced the latter situation are aware that these patients often find it hard to discontinue the drugs.
With benzodiazepines, addiction is relatively low-profile. Moreover, despite the unnoticeable nature of the addiction, the medical side-effects are quite physical and can cause problems for both the patients and for others.
Shantikumar sums up, “What clinicians can do is be aware that they may have patients who have been on these tablets for a long time and are potentially at risk, so it is worth actively thinking about whether a patient needs to continue taking those tablets or if there are alternative strategies. Ultimately, we'd like to specifically identify the individual and GP practice characteristics which may be the driving factors behind long-term benzodiazepine use.”
The optimal outcome, in the view of the investigators, would be to systematically identify those who are using these drugs over the long term, so that their GPs can offer them other options to control their symptoms while reducing the risk of adverse effects and dependence. If anyone thinks they are possibly dependent on these medications, or knows they are addicted, they can get help from their GPs. The researchers also recommend the Frank website for information about the problem as well as locally available addiction services, besides its 24-hour hotline that offers private counseling.
Journal reference:
Socioeconomic status and benzodiazepine and Z-drug prescribing: a cross-sectional study of practice-level data in England. Stephanie Soyombo, Rhian Stanbrook, Harpal Aujla, David Capewell, Mary Shantikumar, Farah Kidy, Daniel Todkill, and Saran Shantikumar. Family Practice. 22 October 2019, cmz054, https://doi.org/10.1093/fampra/cmz054. https://academic.oup.com/fampra/advance-article/doi/10.1093/fampra/cmz054/5601156