The NHS medical evaluation is a preventative initiative that began in 2009 to assess cardiovascular disease risk and aid primary prevention. It detects those who are at risk of developing cardiovascular disease, diabetes, stroke, or renal disease. Healthy individuals aged 40 to 74 years are welcome to their team of primary care physicians for routine physical examinations, health-related inquiries, and blood tests. However, research on the associations of the program with health outcomes and disease prevention efficacy over the long term with follow-up results is limited.
 Study: NHS Health Check attendance is associated with reduced multiorgan disease risk: a matched cohort study in the UK Biobank. Image Credit: doliux / Shutterstock
Study: NHS Health Check attendance is associated with reduced multiorgan disease risk: a matched cohort study in the UK Biobank. Image Credit: doliux / Shutterstock
About the study
In the present observational, case-control study, researchers used the UKBB data to identify individuals who underwent the NHS medical assessment and track new diagnoses during follow-up.
The UKBB included 48,602 medical assessment attendees identified through linked primary-level care data. The team matched the participants on several sociodemographic, medical, and lifestyle covariates to 48,602 individuals who did not have medical assessment records. They obtained diagnoses from medical records over a nine-year follow-up, including diabetes, hypertension, stroke, hypercholesterolemia, myocardial infarction, dementia, heart failure, atrial fibrillation, alcoholic liver disease, fatty liver disorder, liver failure, liver cirrhosis, acute or chronic renal disease, cardiovascular mortality, and all-cause death.
The study sample included 140,899 individuals with seven missing geographical areas or falling below the age range for the health assessment. The team excluded another 20,256 individuals (9.0%) due to pre-existing kidney, liver, brain, or heart diseases. In addition, they excluded 66,135 individuals (31%) due to statin use or a prior history of hypertension or diabetes.
To avoid confounding effects, the team matched one-on-one controls with NHS medical assessment attendees (cases) by closest-neighbor propensity score matching. The team assigned >95% of cases high-quality matches, excluding non-matching individuals. To identify individuals who had undergone an NHS medical assessment, they searched clinical primary care data from April 2006 to December 2022, which yielded 283,536 results. They defined the exposure period as January 1, 2008, to June 30, 2016, with the exposure date being the first reported NHS assessment parameter. They examined existing diseases at baseline using self-reports and data linked with primary care and hospital records.
The study outcomes included hypertension, diabetes, hyperlipidemia, stroke, myocardial infarction, any-cause dementia, atrial fibrillation, cardiac failure, acute or chronic renal disease (stages 3 to 5), alcoholic liver disease, fatty liver disease, liver cirrhosis, hepatic failure, cardiovascular deaths, and any-cause mortality. The team performed Cox survival and aligned-start Cox regression modeling, including all outcomes, excluding outcome events in the first year after the NHS medical evaluation. In the sensitivity analysis, they repeated the aligned-start Cox models with stratified periods.
Results
The study findings showed that in the first two years following the check, health check beneficiaries had higher diagnostic rates for high cholesterol, hypertension, and chronic renal disease than their matched peers. However, over time, NHS medical evaluation beneficiaries had a considerably decreased risk of multiple-organ disease outcomes and lower cardiovascular and any-cause death rates.
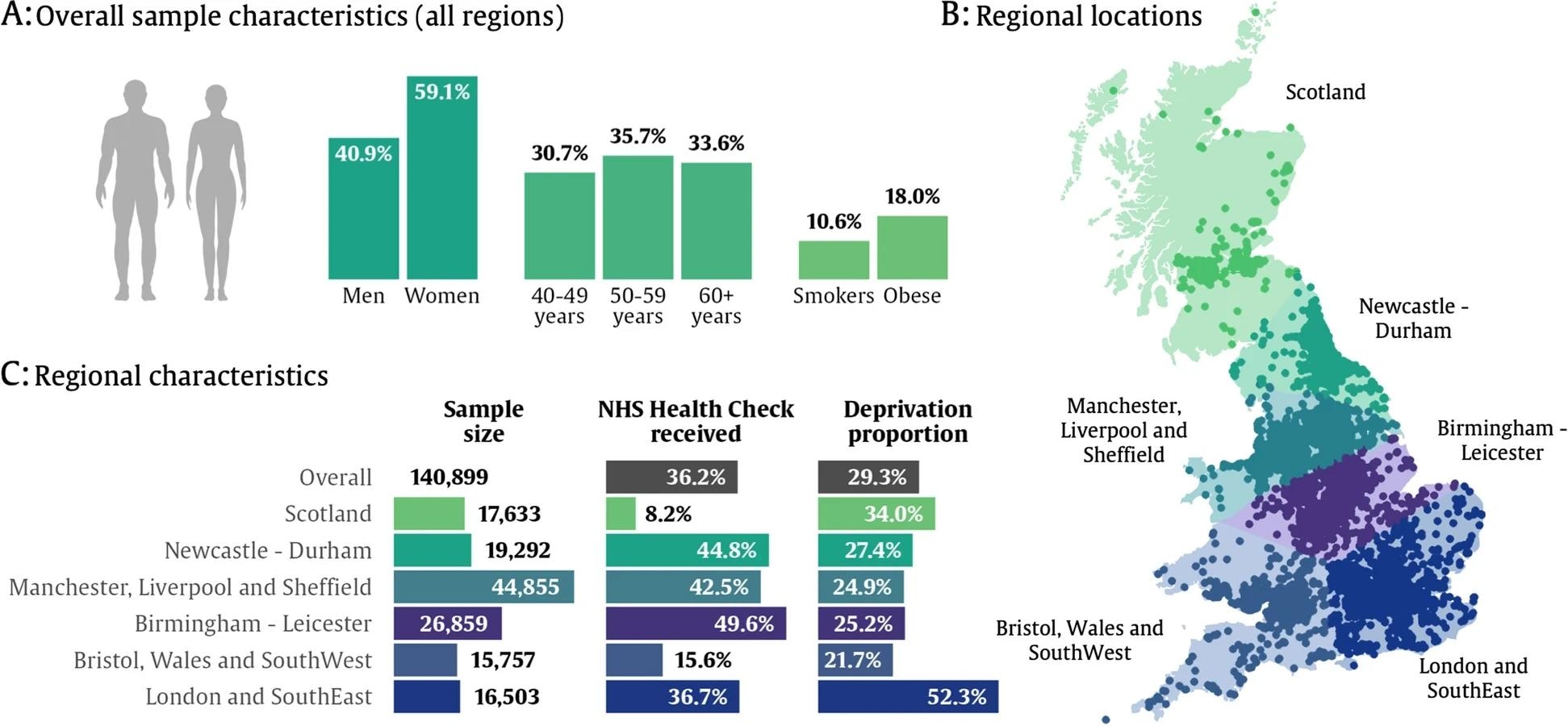 Summary of NHS Health Check in UK Biobank participants. A Overall summaries for the sample of UK Biobank participants with primary care available (n = 140,772). B Summary of geographical locations. C Sample characteristics by geographical region. Deprivation proportion refers to the proportion of the sample that fall above the UK median for socio-economic deprivation according to reported Townsend deprivation scores and quintiles from the 2011 census
Summary of NHS Health Check in UK Biobank participants. A Overall summaries for the sample of UK Biobank participants with primary care available (n = 140,772). B Summary of geographical locations. C Sample characteristics by geographical region. Deprivation proportion refers to the proportion of the sample that fall above the UK median for socio-economic deprivation according to reported Townsend deprivation scores and quintiles from the 2011 census
The sample population (n=140,899) includes 66,573 (47%) individuals who received at least one invitation to an NHS medical evaluation between January 2008 and June 2016. Among the participants, 50,984 (77% of invitees and 36% of the total sample) underwent NHS medical assessments. Most participants received one NHS medical evaluation (88%), whereas 11% received two, and 1.4% received at least three. The study sample was primarily Caucasian, physically active, and consumed alcohol at least once a day.
The team found significant variations in outcomes between cases and controls, including all-cause dementia (1.2% against 1.4%), myocardial infarction (1.9% versus 2.2%), and acute renal injury (4.0% versus 5.3%). Early-event timing effects were less pronounced in regression models with aligned beginnings. Covariate-adjusted modeling showed that NHS medical assessment attendees showed significantly lower rates of dementia due to any cause [19% lower hazard ratio (HR), 0.8], atrial fibrillation (9% lower, HR, 0.9), myocardial infarction (15% lower, HR, 0.85), acute renal damage (HR, 0.8, 23% lower), liver cirrhosis (HR, 0.7, 44% lower), and cardiovascular and any-cause deaths (HR, 0.8, 23% lower).
The study findings showed that the NHS medical assessment is a proactive preventative program that reduces long-term disease outcomes across several organ systems, independent of risk-reducing measures. It reduces cardiovascular and any-cause deaths and the incidence of brain, heart, kidney, and liver disorders. However, it increases the risk of developing chronic renal disease, high cholesterol, and hypertension. Long-term benefits might result from better risk factor detection and treatment, regular reinforcement of healthy behavior, and disease management.