Researchers in the United States have identified mutations within severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) – the agent that causes coronavirus disease 2019 (COVID-19) – that can reduce antibody binding to the virus, potentially mediating its escape from immune attack.
The team used a technique called Phage-DMS to profile this antibody escape in a surface structure called the spike protein, which the virus uses to bind to and infect host cells.
Using blood samples from patients who had recovered from COVID-19, the team tested all possible mutations within the spike protein that might use escape pathways within epitopes that are targeted by convalescent plasma.
The team – from the Fred Hutchinson Cancer Research Center and the University of Washington – found that antibody binding was common in two immunodominant regions, but that there were many unique pathways of escape within these regions.
These escape mutations also differed between individuals, suggesting that antibody binding sites and escape mutants could vary significantly from person to person.
“We identified a spectrum of single mutants that were capable of reducing antibody binding and found person-to-person variability in the effect of mutations within immunodominant epitopes,” writes Julie Overbaugh and the team.
The findings suggest that peoples’ responses to a vaccine that targets the spike protein are unlikely to be uniform, say the researchers.
“In the arms race between the humoral immune response and SARS-CoV-2, these results allow us to predict pathways of escape and forecast the appearance of escape mutants,” writes the team.
A pre-print version of the paper is available on the bioRxiv* server, while the article undergoes peer review.
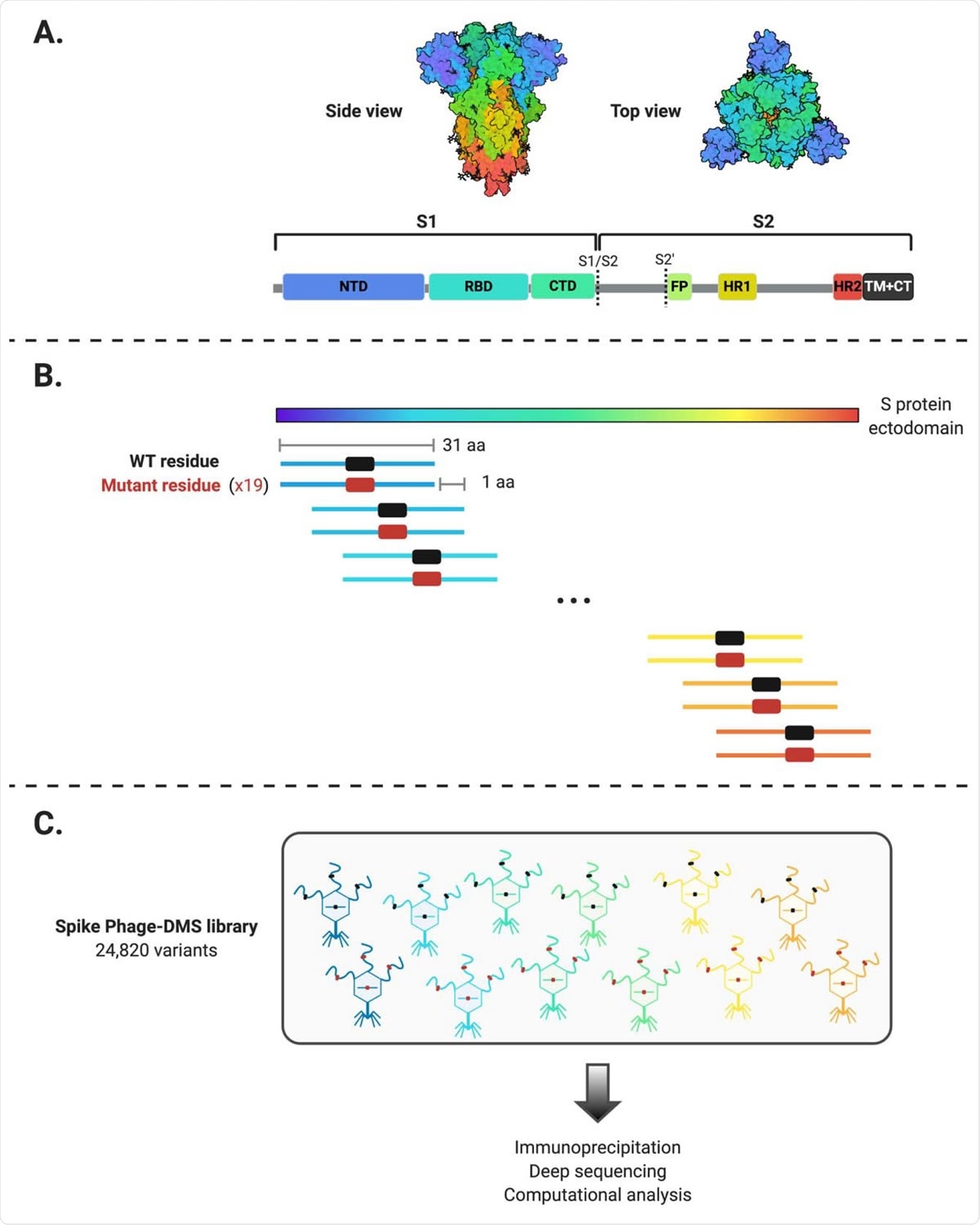
Schematic of the design of the Spike Phage-DMS library. (A) Structure of the S protein and location of important protein domains. Structure was made in BioRender.com (PDB: 6VXX) (B) Sequences were computationally designed to code for peptides 31 amino acids long and to tile stepwise across the Wuhan-Hu-1 SARS-CoV-2 S protein ectodomain by 1 amino acid. There are 20 peptides representing all 20 possible amino acids at the central position, containing either the wild type residue (shown in black) or a mutant residue (shown in red). Within the 31 aa region surrounding the D614G mutation, peptides were also generated with G614 in addition to the 20 amino acid variants at the central position. (C) The designed sequences were cloned into a T7 phage display vector and amplified to create the final S protein Phage-DMS library. This library was then used in downstream immunoprecipitation and deep sequencing experiments with human plasma.

 This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
Researchers are uncertain whether SARS-CoV-2 immunity is long-lasting
Determining whether immunity to SARS-CoV-2 can be protective in the long-term is one of the most pressing challenges faced by researchers working to develop vaccines against SARS-CoV-2.
Understanding how the virus could potentially evolve to escape immune protection is crucial to answering this question.
The main viral target of interest to researchers is the spike protein – the structure that initiates host cell binding and fusion to enable viral entry.
The spike protein is made up of two subunits. Subunit 1 (S1) contains an N-terminal domain (NTD) and a receptor-binding domain (RBD). Subunit 2 (S2) contains a fusion peptide (FP) and two heptad repeat regions (HR1 and HR2), separated by a linker region, that drive virus and host membrane fusion.
Once S1 binds to a host cell via the RBD, proteolytic cleavage occurs within S2 that exposes FP and triggers a series of conformational changes that enable membrane fusion.
Neutralizing antibodies that target the RBD have been the main focus of efforts to develop vaccines and antibody therapies. These neutralizing antibodies have been shown to block viral entry in vitro and to prevent infection or disease in preclinical models.
“However, the study of other coronaviruses has illustrated that antibodies elicited by infection can target epitope regions outside of the RBD,” say Overbaugh and colleagues. “Thus, there may be multiple regions within the SARS-CoV-2 spike protein that may shape the viral immune response.”
Furthermore, given the unusually high transmission rate of SARS-CoV-2 and the high mutability of previous coronaviruses, variants that are capable of evading the immune response are likely to arise.
What did the researchers do?
Previously, Overbaugh and the team developed a method called Phage-DMS to comprehensively map escape mutations that enabled HIV to avoid binding by monoclonal antibodies.
The team has now used this technique to identify mutations in the SARS-CoV-2 spike protein that could reduce antibody binding and, therefore, mediate escape from antibodies present in the plasma of COVID-19 patients.
What did they find?
The team found that antibody binding was common in two regions: the FP and the linker region upstream of HR2.
The study revealed a spectrum of single mutants that were capable of reducing antibody binding within these regions.
However, the escape mutations showed variability within these immunodominant regions, as well as person-to-person variability.
What are the implications of the study?
The findings suggest that the pattern of virus evolution is not likely to be driven by a single antibody escape mutation. They also suggest there will be between-individual variation in antibody-mediated evolution of the virus.
“Thus, the responses to a SARS-CoV-2 spike protein vaccine are not likely to be uniform, nor will the pathways of escape,” writes the team.
The researchers say the FP and linker region/HR2 epitopes could serve as alternative targets for vaccine and immunotherapy development that could complement efforts focused on the RBD.
The team says that S2 overall, especially the FP, is highly conserved in coronaviruses. These more conserved regions could be important targets for the design of optimal and durable vaccines.
“These studies have defined common and variable escape mutations across COVID-19 patients that will be useful for viral surveillance, particularly as SARS-CoV-2 spike protein-based vaccines are introduced into the population,” write the researchers.
Furthermore, the spike protein Phage-DMS library used in this study could be used to examine larger cohorts, potentially including individuals of varying ages and with variable clinical outcomes, suggest Taylor and colleagues.
This could help to “define whether mutations that disrupt antibody binding vary in a systematic way across populations and whether this is correlated with clinical outcome or risk of reinfection,” concludes the team.

 This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
Journal references:
- Preliminary scientific report.
Overbaugh J, et al. High resolution profiling of pathways of escape for SARS-CoV-2 spike-binding antibodies. bioRxiv, 2020. doi: https://doi.org/10.1101/2020.11.16.385278, https://www.biorxiv.org/content/10.1101/2020.11.16.385278v1
- Peer reviewed and published scientific report.
Garrett, Meghan E., Jared Galloway, Helen Y. Chu, Hannah L. Itell, Caitlin I. Stoddard, Caitlin R. Wolf, Jennifer K. Logue, et al. 2021. “High-Resolution Profiling of Pathways of Escape for SARS-CoV-2 Spike-Binding Antibodies.” Cell 184 (11): 2927-2938.e11. https://doi.org/10.1016/j.cell.2021.04.045. https://www.cell.com/cell/fulltext/S0092-8674(21)00580-8.