In a recent study published in the journal Nature, researchers investigated the influence of paternal gut microbiota perturbations on offspring health in mice. They found that dysbiosis in the paternal gut microbiota affects placental function, increasing the likelihood of growth restriction, low birth weight, and premature mortality in the offspring. Further, they found that the transmission of disease risk occurred via the germline and could be rescued by restoring the father's microbiota before conception.
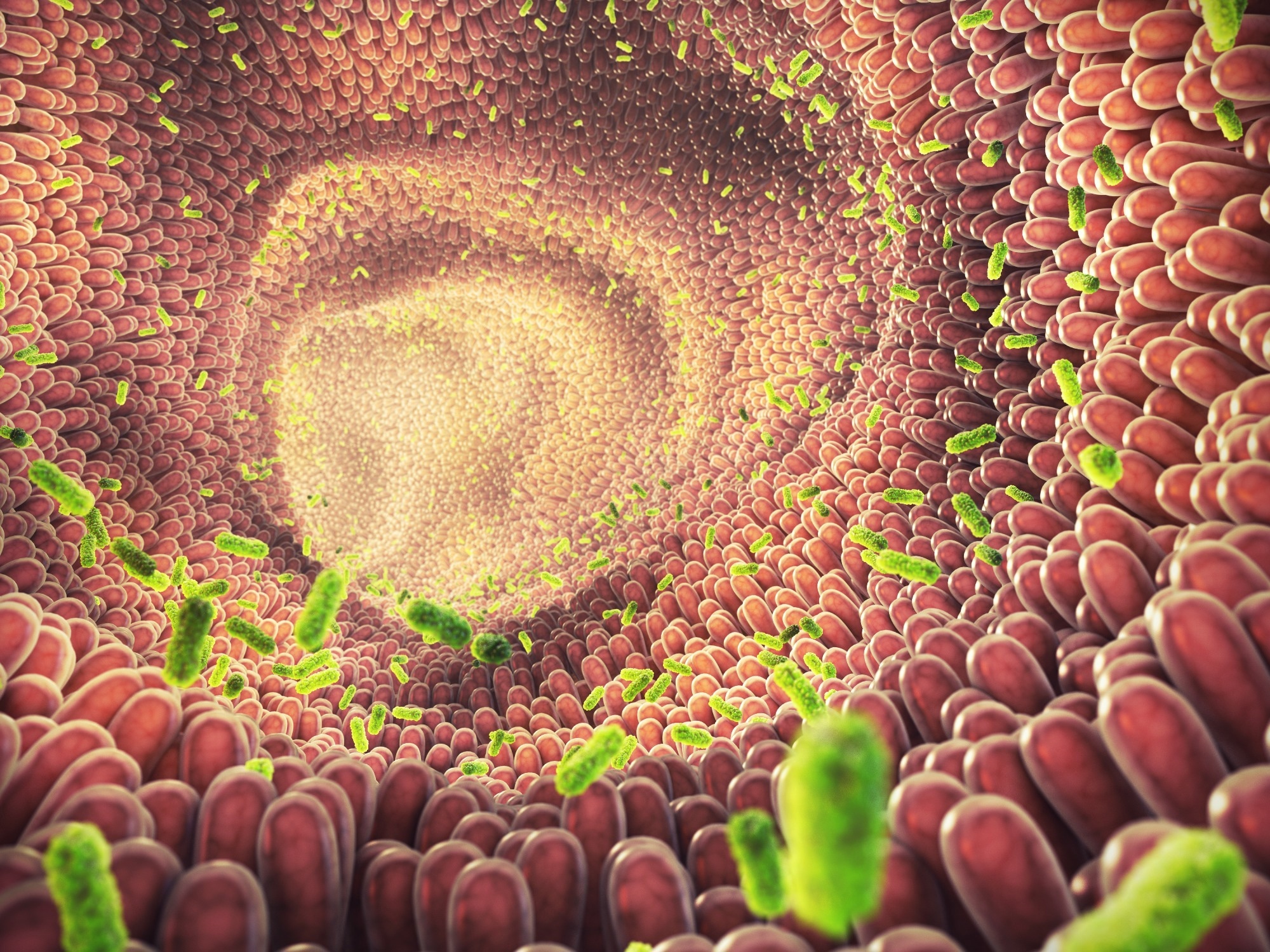 Study: Paternal microbiome perturbations impact offspring fitness. Image Credit: nobeastsofierce / Shutterstock
Study: Paternal microbiome perturbations impact offspring fitness. Image Credit: nobeastsofierce / Shutterstock
Background
Sperms carry both genetic and epigenetic information to the next generation, with the latter influenced by the preconception environment. While the extent and mechanisms of paternal epigenetic effects in mammals are not fully understood, the gut microbiota plays a crucial role in integrating environmental signals into host responses. Environmental factors like diet and medication shape gut microbiota composition, and an imbalance in it (dysbiosis) is shown to trigger physiological responses across tissues. However, the impact of dysbiosis on the germline remains largely unexplored, highlighting a gap in our understanding of the interplay between environmental factors, microbiota, and heritable traits. Therefore, in the present study, researchers examined the effect of induced imbalance in the paternal gut microbial diversity on health outcomes in the offspring.
About the study
In the study, male mice were treated with non-absorbable antibiotics (nABX), an alternative combination of antibiotics (avaABX), or osmotic laxatives (polyethylene glycol - PEG) for six weeks to induce microbiota dysbiosis. They were then mated with untreated females, and F1 offspring phenotypes were scored and analyzed. Severe growth restriction (SGR) was quantified based on body-weight Z-scores and SGR-offsprings were analyzed by transcriptional profiling. Testes of the dysbiotic fathers were analyzed for size, sperm count, histological changes, and leptin levels. Deoxyribonucleic acid (DNA) methylation and small ribonucleic acid (sRNA) profiling were conducted on sperms.
Further, transcriptomic analysis was performed on embryos and placentae at E13.5 (mid-gestation) and E18.5 from matings with nABX-treated males. Placental structure and markers of placental insufficiency were assessed. The potential for paternal recovery from gut dysbiosis to rescue F1 phenotypic effects was studied via nABX withdrawal for eight weeks and further analysis.
Results and discussion
As per the study, offspring (male or female, n = 181) sired by nABX-treated fathers showed significantly lower neonatal birth weight compared to offspring from control fathers (n = 172). The mean body weight of F1 offspring from nABX-treated males remained significantly lower throughout postnatal development. Additionally, they showed higher odds of SGR and increased postnatal mortality rates, especially among those with SGR. SGR offsprings from independent nABX-treated males showed consistent transcriptional profiles, distinct from offspring of control sires. Analysis revealed enrichment of genes related to metabolic processes, particularly lipid metabolism, supporting an intergenerational impact of paternal dysbiosis on offspring growth, metabolism, and survival. Further, paternal administration of avaABX or PEG also showed an increased risk of reduced body weight, SGR, and premature mortality in the progeny. These findings suggest a direct association between induced paternal dysbiosis and offspring health outcomes. Interestingly, these effects were found to reverse upon paternal microbiome recovery. F1 phenotypes were found to majorly arise from paternal gametes and associated molecules, with no significant transmission of altered microbiota to mother or offspring.
Dysbiotic males had smaller testes, reduced sperm count, structural abnormalities, reduced leptin levels, and altered testicular metabolites and gene expression patterns. Leptin-deficient mice displayed similar testicular abnormalities and transmitted altered gene expression to offspring. Sperms from dysbiotic males showed changes in sRNA composition. The results indicate that induced microbiome dysbiosis leads to systemic dysregulation of leptin. Additionally, perturbation of paternal leptin levels before conception affects offspring gene expression patterns, highlighting leptin's role in the "gut-germline axis" and its intergenerational impact.
In the transcriptomic analysis, embryos showed no DEGs at E13.5, but placental transcriptomes had 538 DEGs, including downregulated factors crucial for placental development. At E18.5, placental transcriptomes continued to differ based on paternal microbiome status, with 348 DEGs linked to steroid metabolism and glycolysis. Placentae from dysbiotic fathers displayed reduced mass and structural abnormalities resembling placental insufficiency disorders like preeclampsia. Key preeclampsia markers, like placental growth factor (PLGF) and the soluble fms-like tyrosine kinase 1 (sFLT)/PLGF ratio, were dysregulated in placentae from offspring sired by dysbiotic fathers.
Conclusion
In conclusion, the study suggests that perturbations in prospective fathers' gut microbiota can lead to significant reproductive responses and affect offspring disease risk through placental function. This implies the existence of a regulatory gut-germline axis through which environmental inputs, like antibiotics or diet, can influence male germ cells and subsequently impact progeny. The reversibility of these effects through the restoration of paternal gut microbiota before conception offers potential avenues for remediation, especially with lifestyle and antibiotic practices currently shaping human microbial communities. Overall, while the underlying mechanisms need to be further explored, the findings highlight the role of environmental factors in the modulation of complex biological systems and intergenerational disease susceptibility.