As COVID-19 pandemic continues to unfold, researchers worldwide are rushing to carry out and report novel insights in order to understand how the virus works and how the disease can be treated, but even more importantly, what is the exact risk of infection or death.
Consequently, different risk factors have been reported concerning COVID-19 morbidity and mortality. These include male sex, age over 65, and a history of smoking, as well as underlying diseases such as high blood pressure, diabetes, and various respiratory conditions.
However, some studies have recently described a relationship between the ABO blood group system and COVID-19 morbidity/mortality. Previously, the ABO blood group system has been linked to different infectious diseases and respiratory syndromes, such as influenza, SARS, norovirus, Helicobacter pylori, acute respiratory distress syndrome, and acute hypoxemic respiratory failure.
Still, for COVID-19, the reported results are considered controversial. Therefore, the research group from the Mazandaran University of Medical Sciences (Sari), Zabol University of Medical Sciences (Zabol), and Universal Scientific Education and Research Network (Tehran) in Iran aimed to perform a rapid (but comprehensive) systematic review and meta-analysis to unveil any purported association between the ABO blood group system and COVID-19 infection/death risk.
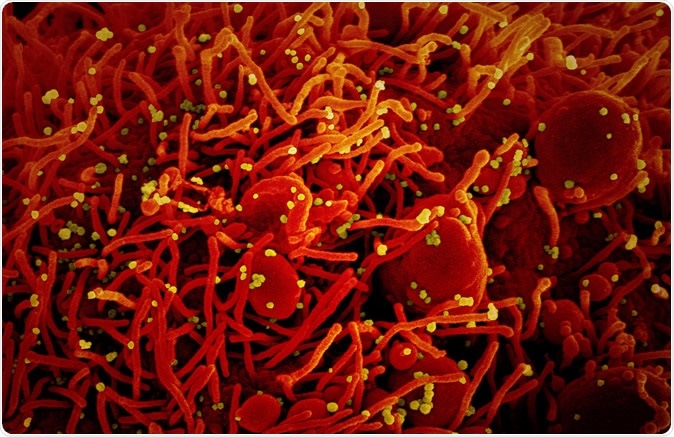
Novel Coronavirus SARS-CoV-2 Colorized scanning electron micrograph of an apoptotic cell (red) infected with SARS-COV-2 virus particles (yellow), isolated from a patient sample. Image captured at the NIAID Integrated Research Facility (IRF) in Fort Detrick, Maryland. Credit: NIAID
Digging out the important findings
A systematic literature appraisal was carried out across the most relevant research databases – Including Scopus, PubMed, Web of Science, Cochrane library – but also in preprint servers such as medRxiv. All cohort, cross-sectional and case-control studies published until April 21, 2020, were included in this paper, while case-reports and letters to the editors were excluded.
Quality assessment was performed with the use of The Newcastle-Ottawa Scale (NOS), which is commonly employed in meta-analyses. This checklist contains three parts: selection, comparability, and exposure. As the checklist scores are within a range from zero to nine, studies with a score lower than five were excluded.
Only four studies passed strict scientific criteria posed by this study; more specifically, the eligible papers that were included in the final statistical analysis were two case-control studies, one cohort study, and one cross-sectional study.
The estimated frequency of COVID-19 morbidity and mortality in terms of ABO blood group and estimated odds ratio across the blood groups with COVID-19 infection and death was done by using a 95% confidence interval. Study heterogeneity was assessed by utilizing Cochrane's Q test (traditionally used for meta-analyses) with the additional support from I-squared and other statistical techniques.
Blood group A associated with a higher risk of COVID-19 infection
The pooled frequencies for blood groups A, B, 0, and AB among COVID-19-infected individuals were estimated at 36%, 25%, 30%, and 9%, respectively. In addition, frequencies of blood groups A, B, 0, and AB among those who died due to COVID-19 infection were estimated at 40%, 23%, 29%, and 8%, respectively.
In a nutshell, the researchers found that blood group A carries a partial risk factor for COVID-19 infection (odds ratio of 1.16), while blood group O was actually a protective factor (odds ratio of 0.73). Furthermore, B and AB blood groups were not significantly associated with COVID-19 infection.
When mortality is considered, there were no statistically significant associations between blood groups and COVID-19. This suggests other factors still predominate in driving up mortality rates, most notably when there is a high susceptibility to respiratory failure due to a plethora of pathophysiological mechanisms.
The need for further studies
Although this meta-analysis hinted that individuals with blood group A carry a higher risk for COVID-19 infection, no statistically significant relationship was found between the blood group and mortality from COVID-19, which is otherwise known to strike the elderly, obese and those with underlying illnesses.
"Although we didn't find a statistically significant relationship between blood group A and COVID-19 mortality, one study suggests higher mortality among blood group A individuals", say study authors. "It might be because of failure of pulmonary microcirculation and the higher risk of thrombosis in blood group A, as microthrombi have been seen in lungs and kidneys," they add.
Further studies are warranted in order to understand the exact relationship between blood groups and COVID-19 mortality. Clinical risk profiling of patients with COVID-19 and targeted exploration of severe disease pathophysiology remain crucial steps for successfully tackling this pandemic.

 This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources