In a recent report published in the Morbidity and Mortality Weekly Report (MMWR), the United States (US) Centers for Disease Control and Prevention (CDC) shares its recommendations for the tests and protocols required to diagnose syphilis in the US. The recommendations build upon existing conventional serologic algorithms and involve the combined use of nontreponemal and treponemal tests to identify if the patient’s immune response indicates a current untreated infection or a past-treated one. Additionally, recommendations for the direct microscopic detection of Treponema pallidum, the causative pathogen of syphilis, are included. These recommendations will help clinical laboratory directors, clinicians, laboratory staff, disease control personnel, and patients combat this dreadful disease.
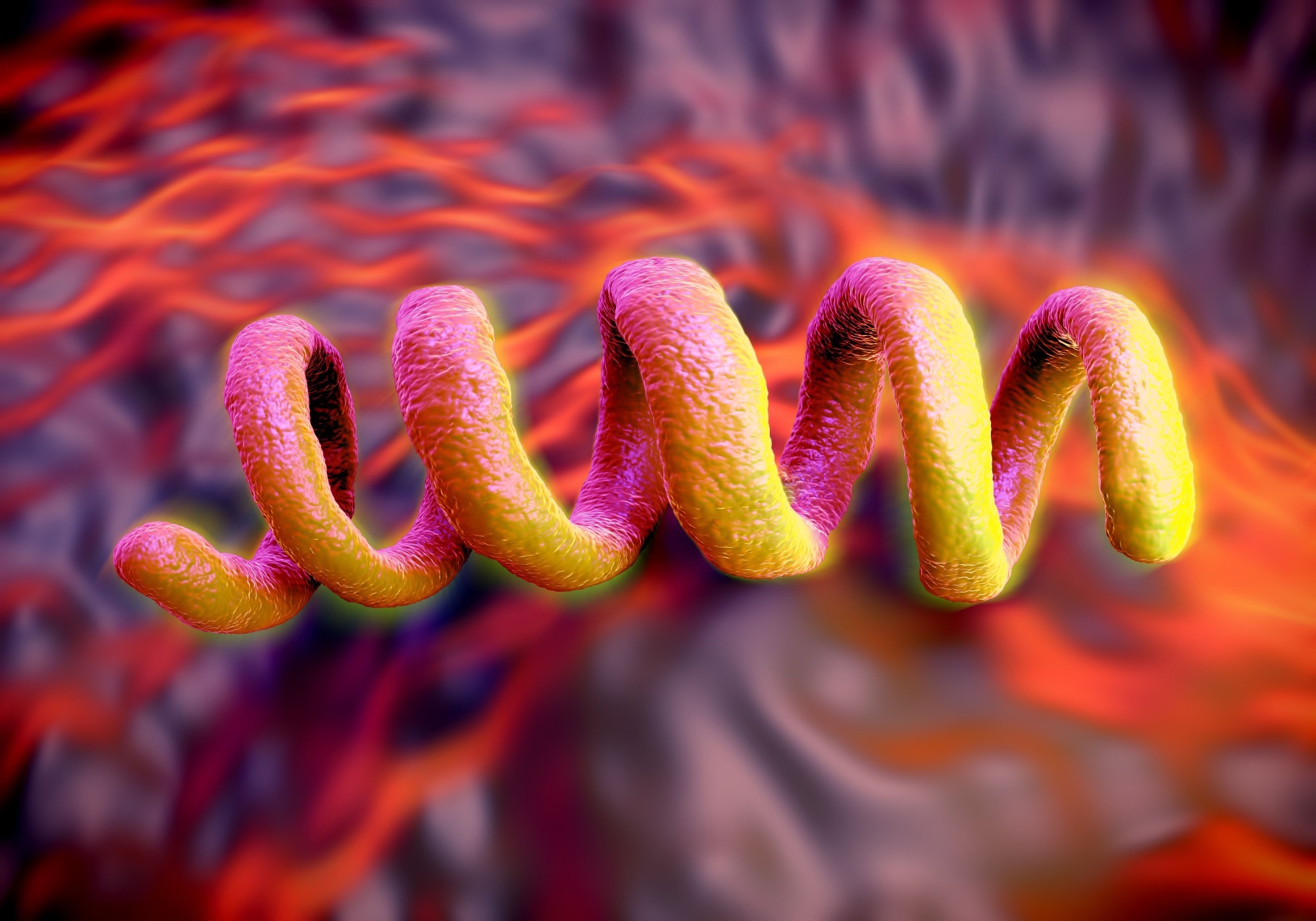 CDC Laboratory Recommendations for Syphilis Testing, United States, 2024. Image Credit: Peddalanka Ramesh Babu / Shutterstock
CDC Laboratory Recommendations for Syphilis Testing, United States, 2024. Image Credit: Peddalanka Ramesh Babu / Shutterstock
Why do we need these recommendations?
Syphilis is a bacterial sexually transmitted infection (STI) that progresses in stages from a painless sore (stage 1) to a severe disease that may attack the brain, liver, nerves, eyes, or cardiovascular system (stage 3). Caused by the bacterium Treponema pallidum subspecies pallidum, the disease has been further associated with congenital complications such as stillbirths, spontaneous abortions, and miscarriages.
Alarmingly, the global burden of syphilis is rising rapidly, especially in wealthy and developed countries, with approximately 6 million new cases in 2021 alone. Reports from the United States of America (US) observe an increase of 2,140% in syphilis incidence rates between 2000 (n = 5,979) and 2020 (n = 133,945), suggesting a local epidemic within the country. Research has characterized this epidemic as displaying significant health disparities, with gender and sexual minorities being the worst affected.
The laboratory diagnosis of syphilis represents a crucial effort in the war against the disease. Timely diagnoses, especially before the onset of stage 3 syphilis, are critical for positive disease outcomes. Public health reporting by laboratories provides the Centers for Disease Control and Prevention (CDC) and other government agencies the information needed to enact policies to attenuate local outbreaks and monitor epidemic trends.
About the report
The current report details the CDC’s first-ever recommendations for syphilis testing and includes optimal methods for point-of-care (POC) tests, laboratory-based tests, sample processing, and reporting. These recommendations were formulated by CDC scientists in collaboration with the Association of Public Health Laboratories (APHL) after reviewing up-to-date peer-reviewed literature, especially publications published by the US Food and Drug Administration (FDA).
Serologic Laboratory Testing
The first section of the report summarises progress in syphilis serological testing since the invention of the Wassermann test through to current nontreponemal (lipoidal antigen) and treponemal tests. In brief, when patients display symptoms or signs of syphilis or have had known sexual contact with a diagnosed syphilis patient, nontreponemal (lipoidal antigen) tests are recommended for laboratory screening. These tests are also recommended when assessing reinfections or reporting outcomes during clinical trials.
“Nontreponemal (lipoidal antigen) tests might be less sensitive than treponemal tests in early primary syphilis and tend to wane with time regardless of treatment. Before testing, test and specimen type should be carefully considered because serum and plasma cannot always be used interchangeably, and certain nontreponemal (lipoidal antigen) tests require heat treatment of specimens. One caveat of nontreponemal (lipoidal antigen) tests is that a reactive result could be a false positive because of recent conditions (e.g., infections, vaccinations or injection drug use, or underlying autoimmune or other chronic conditions).”
Nontreponemal tests are usually carried out manually, but some test versions (e.g., the rapid plasma reagin [RPR] test) may be automated to increase throughput. In the latter (automated) case especially, care must be taken to ensure that samples are maintained at optimal conditions and coinfections are accounted for to ensure diagnostic performance and prevent false positives. Treatment outcomes are best reported by comparing nontreponemal antibody titers at baseline and 12 months following treatment, at which time titers are expected to reduce fourfold.
Treponemal tests are used to validate nontreponemal test results and to diagnose early syphilis infections that cannot (yet) be detected by nontreponemal tests. Most of these tests are conducted manually, but some can be automated for high throughput. In most patients, treponemal antibodies are detectable for life and are helpful to indicate a past, successfully treated syphilis infection. All donations to blood banks must undergo treponemal screening to ensure that volunteered blood is free of syphilis antibodies.
Syphilis screening algorithms
The traditional algorithm for syphilis screening involved nontreponemal tests followed by treponemal tests to confirm any dubious or contentious nontreponemal results. This is because the former is comparatively inexpensive and rapid, while the latter is manually labor-intensive, expensive, and limited in number. However, recent advancements in automated treponemal immunoassays have bridged the time and monetary gap between these techniques, resulting in the more recent ‘reverse’ algorithm for syphilis screening, wherein nontreponemal tests are used to validate the results of treponemal tests further.
Building upon these methodologies, the report provides recommendations for the optimal screening, clinical care, and recording of patients suffering from neurosyphilis, ocular syphilis, otosyphilis, and congenital syphilis. Pregnancy status, in particular, is noted as a condition that should not influence the standard interpretation of nontreponemal and treponemal test results due to scientific evidence that their functioning is not altered during pregnancy.
Direct detection tests
Immunohistochemistry and microscopy techniques for detecting syphilis from biopsies and other preserved samples are outlined with a particular focus on darkfield microscopy (the most widely used method for direct syphilis detection) and silver staining. Darkfield microscopy has been found to outperform antibody screening approaches, especially in the early stages of infection, thereby presenting itself as an ideal tool for early disease detection.
While Nucleic Acid Amplification Tests (NAATs) have shown great potential in accurately diagnosing syphilis infection, no FDA-approved NAATs currently exist. These recommendations are expected to be updated once FDA-approved NAATs enter the market.