The SARS-CoV-2-induced coronavirus disease 2019 (COVID-19) is a highly contagious viral illness that has claimed the lives of more than 7 million humans and infected almost 100 times that number since its discovery in late 2019. The resulting pandemic has severely impacted global healthcare, economy, and infrastructure. Alarmingly, more than 60% of COVID-19 survivors display persistent symptoms even months or years following primary infection recovery, significantly hampering their quality of life. Furthermore, acute SARS‑CoV‑2 infections have been associated with several comorbidities, most of which remain relatively unexplored.
Sensory (mainly olfactory and auditory) and cognitive impairments are some of the most commonly reported comorbidities of COVID-19. Unfortunately, while a growing body of research aims to explore sensory pathophysiology, the neurological impacts of COVID-19 are hitherto a mystery despite almost 33% of all COVID-19 patients displaying cognitive loss. Most research in the field remains observational, and thus far, scientific knowledge is restricted to SARS-CoV-2 causing encephalopathy and delirium in some of its survivors. The limited number of studies into COVID-19-associated neuropathology use suboptimal metrics to assess cognition and entirely exclude examinations of biological substrates.
Understanding potential COVID-19-associated brain injury and structural modifications requires high-resolution neuroimaging in tandem with assessments of neurological biomarkers. These tools would allow for the elucidation of post-acute (more than three months following severe SARS‑CoV‑2 infection) pathophysiological evaluations, thereby providing the first step in improving the quality of life for patients with ongoing cognitive symptoms.
About the study
The present study aims to improve scientific understanding of COVID-19-associated neuropathology by comparing neurological biomarkers and high-resolution neural scans between acute COVID-19 patients (requiring hospitalization) and healthy controls. The study cohort was derived from the COVID-19 Clinical Neuroscience Study (COVID-CNS), a prospective, United Kingdom (UK)-based study conducted by the National Institute of Health Research (NIHR) aimed at elucidating the psychiatric and neurological complications of COVID-19.
Study inclusion criteria comprised age (16 years and older), hospitalization (for the case-cohort), and no prior neurological diagnoses. Data collection included anthropometrics and demographics (age, sex, clinical frailty status, ethnicity, and epoch of COVID-19 infection) and medical reports (COVID-19 infection severity and neurological/psychiatric evaluations). Cases were matched to eight controls selected to mirror the age, sex, ethnicity, and epoch of infection cases as closely as possible.
Study-specific cognitive assessment was carried out using three rounds of the Cognitron assessment battery, with the first round comprising in-person supervised evaluation and the following two rounds online.
“Cognitive tasks were selected to sample across five domains defined by the DSM-5 classification (45) - Executive Function; Learning and Memory; Complex Attention; Perceptual-Motor Control and Language. Accuracy and median RTs were extracted by task, comprising 13 measures.”
Serum collected from study participants was used for brain injury biomarker assessments, taking readings from 60 healthy volunteers (from the NIHR BioResource) as the normative baseline values. 3.0 Tesla magnetic resonance imaging (3T MRI) was used for neuroimaging and consisted of scans from the parahippocampal gyrus, entorhinal cortex, anterior cingulate cortex, insula, orbitofrontal cortex, and superior temporal gyrus.
Statistical analyses comprised linear models comparing cases and controls, corrected for demographic characters.
Study findings
Three hundred and fifty-one cases and 2,927 controls met the study inclusion criteria and comprised the study cohort. Neurological evaluations revealed that Cognitron scores were significantly lower in cases compared to controls across all five measured domains, with cases displaying encephalopathy scoring the lowest across cohorts. Cognitive accuracy and response times were substantially lower than baseline expectations, irrespective of SARS‑CoV‑2 infection severity.
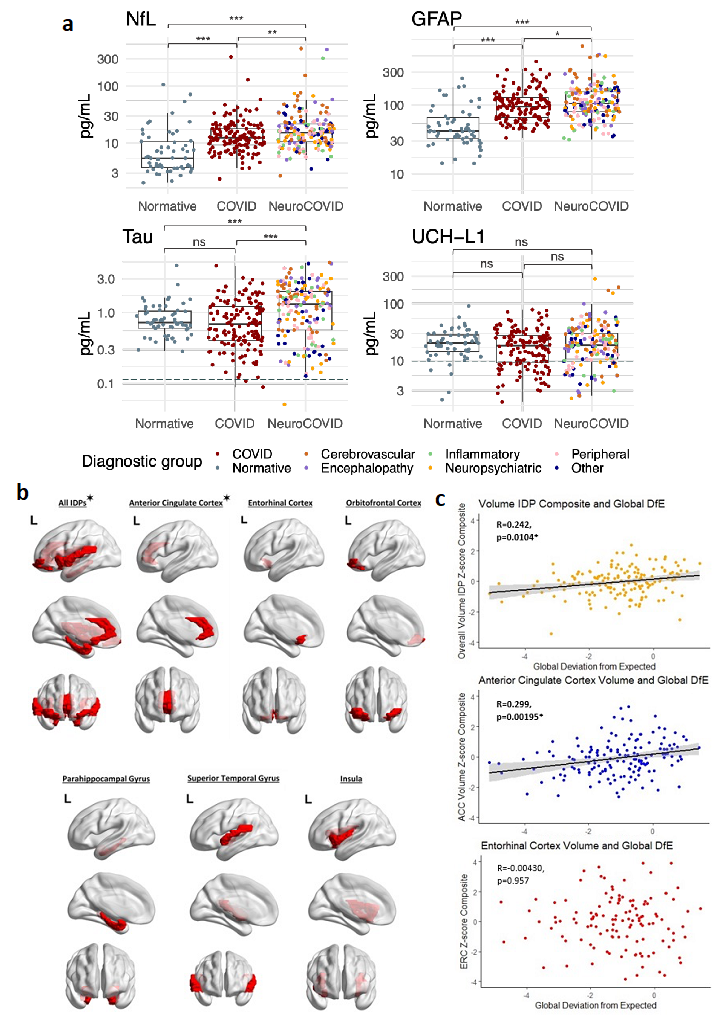
a: Brain injury markers in pg/mL by diagnostic group. Lower limit of quantification (LLOQ marked (dashed)) if included in scale. Normative values from n=60 healthy controls. * p < 0.05, **p < 0.01, ***p < 0.001, ns= non-significant. b: Brain regions represented by the image derived phenotypes (IDPs) utilised in analyses. These regions are parcellated as per the Desikan-Killiani cortical atlas. For each region and regions combined, IDP composites for thickness and volume were utilised. ✶= IDP composites that have significant correlations with overall cognition (Supplementary Table 3). Created using Matlab and BrainNet Viewer (54). c: Scatter plots for IDP composite z-scores against global deviation from expected in the overall cohort, with trend line in black and 95% confidence interval in grey. Significance persisting after False Discovery Rate correction for multiple comparisons
Alarmingly, follow-up assessments revealed that cognitive recovery took months and, in some cases, remained incomplete. Early epoch SARS‑CoV‑2 infections were associated with the most prolonged recovery durations and the highest incomplete recovery risk.
Biomarker assessments depicted that serum neurofilament light chain and glial fibrillary acidic protein, both biomarkers of brain injury, were significantly higher in patients with prior SARS‑CoV‑2 infections compared to healthy controls. Even amongst COVID-19 patients, Tau proteins were upregulated, corresponding to the degree of observed cognitive impairment.
One-way analysis of variance (ANOVA) of composite image-derived phenotype (IDP) z-scores revealed reductions in brain thickness and volume between case and control cohorts. Given that SARS-CoV-2 rarely invades the brain, these results suggest that brain injury is immune-mediated.
Conclusions
The present study presents the first formal investigation into the pathophysiology of COVID-19-associated cognitive impairment using both biomarkers and high-resolution neuroimaging. Comparisons between 351 acute COVID-19 patients and 2,927 healthy controls across cognitive, biomarker, and neuroimaging assessments reveal that COVID-19 significantly and globally impacts neurological function via measurable brain injury and loss in brain thickness and volume. These results suggest that injury in moderate to severe SARS‑CoV‑2 infection is immune-mediated.
“However, care needs to be taken in both inferring cause and effect, and extrapolating these results to a broader COVID-19 population. Mechanisms underpinning this potentially immune-mediated construct of depression, cognition and brain injury need to be further elucidated, to allow the development of targeted therapeutic interventions.”

 *Important notice: Research Square publishes preliminary scientific reports that are not peer-reviewed and, therefore, should not be regarded as conclusive, guide clinical practice/health-related behavior, or treated as established information.
*Important notice: Research Square publishes preliminary scientific reports that are not peer-reviewed and, therefore, should not be regarded as conclusive, guide clinical practice/health-related behavior, or treated as established information.