Over 68.74 million people around the world have been infected with severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), the causative pathogen for coronavirus disease 2019 (COVID-19). The infection has already killed over 1.56 million people globally, and thrombotic complications and increased blood coagulation are among the leading causes of worsening of patients with COVID-19. These thrombotic complications are also one of the major causes of death among hospitalized patients.
Background
The SARS-CoV-2 infection was initially thought to be an exclusively respiratory illness. After the pandemic was declared by the World Health Organization (WHO) on the 11th of March 2020, it was soon found that patients developed thrombotic complications or problems associated with increased coagulation.
The researchers explained that both platelets and neutrophils in the blood are activated in COVID-19 patients. The team says that SARS-CoV-2 infection is commonly associated with an increased propensity for blood clotting – a condition called hypercoagulability. This leads to one of the common complication called venous thromboembolism (VTE). For this study, the team analyzed platelet and neutrophil activation in COVID-19 patients and the link of this activation with VTE.
COVID-19 associated thromboembolism
Apart from venous thromboembolism (VTE), COVID-19 patients also were seen to develop arterial and microvascular thrombosis. The authors of the study explain that evidence shows that widespread inflammation within the body is one of the major causes of this pathology.
The team writes, "abnormal coagulation parameters and high concentrations of proinflammatory cytokines are associated with disease severity, poor prognosis and with the incidence of VTE in COVID-19 patients".
Those with low platelet counts or thrombocytopenia as well as raised neutrophil counts also developed these complications, the team writes. These patients were more likely to have severe disease and be admitted with complications. This shows that "blood cells are deeply involved in the evolution of the infection," write the researchers.
Inflammation and platelets
When there is a viral infection, the platelets are the first to be activated, and there are significant interactions between activated platelets and neutrophils. The team writes, "platelets act as blood sentinels quickly detecting invading pathogens through pattern recognition receptors (e.g., TLRs), get activated and form platelet-neutrophil complexes." The activated neutrophils release microparticles (PMN-MPs) that lead to thrombosis in "vasculitis, inflammatory bowel disease and acute coronary syndromes," the team explains.
Study design
To date, no studies have looked at the PMN-MPs in COVID-19 patients. This study looked at the platelet and neutrophil activation along with "MMP-9 (matrix metalloproteinase-9) and MMP-9/NGAL levels" in COVID-19 patients. The team also attempted to check if common antithrombotic agents could prevent COVID-19 related complications. They checked if these drugs could stop the patient's plasma-triggered platelet and neutrophil activation and NET (neutrophil extracellular traps) formation in vitro as well.
A total of 36 COVID-19 patients were included. Participants included hospitalized COVID-19 patients and age- and sex-matched healthy participants as controls. For the participant samples, the team measured platelet and leukocyte activation, NET formation, MMP-9 release. MMP-9 is an enzyme released by the neutrophils. Patients were observed again after recovering from the infection.
Then the team looked at the activating effect of COVID-19 plasma from the patients on the control samples with platelets and leukocytes and checked if the common antithrombotic agents could stop this activation.
Findings
Results showed that 22.2 percent or 8 of 36 patients developed VTE. Platelets and neutrophils were found to be activated in all patients.
Significant NET but not platelet activation associated with severe disease was also observed. The NET was a biomarker associated with disease severity and thrombosis, the team found. Plasma levels of MMP-9 were significantly increased in COVID-19 patients. MMP-9 is released by the neutrophils. Platelet and neutrophil activation markers again fell to normal levels after recovery, the 4 patients studied after recovery revealed.
In vitro, plasma from COVID-19 patients was found to trigger the platelet and neutrophil activation and NET formation. A standard antithrombotic agent used low molecular weight heparin (LMWH), was then found to block the activation of the neutrophils and platelet activation. Similar protective effects were not seen with aspirin or dypiridamole.
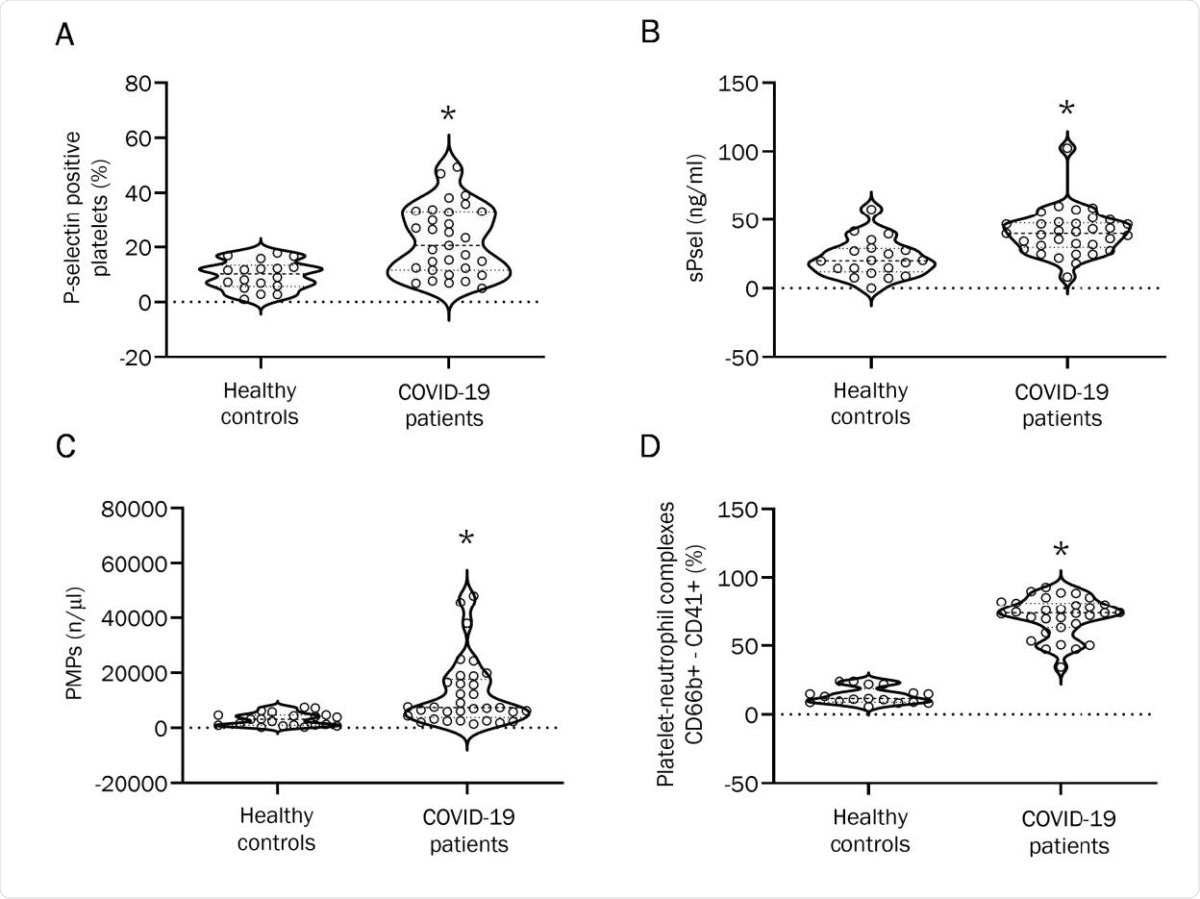
Effect of COVID-19 plasma on platelets and neutrophils from healthy controls. (A) Platelet surface P-selectin expression in whole blood of healthy controls mixed with plasma from healthy controls or from COVID-19 patients. Results are reported as percentage of positive cells. (n=6; *p<0.05). (B) CD66b+-CD41+ complexes in whole blood of healthy controls stimulated by plasma from healthy controls and from COVID-19 patients. Results are reported as percentage of positive cells. (n=9; *p<0.01). (C) MPO-DNA complex formation upon mixing with plasma from healthy controls or from COVID-19 patients (n=11 healthy controls, n=15 COVID-19 patients; *p<0.05). (D) Plasmatic levels of MMP-9 upon mixing with plasma from healthy controls or from COVID-19 patients (n= 12; *p<0.05).
Conclusions and implications
This study reveals that both platelets and neutrophils are activated in COVID-19 patients but raised neutrophil extracellular trap (NET) biomarkers are more important markers associated with severe evolution and thrombotic events. These markers can also help to predict clinical worsening and VTE. This study also shows that low molecular weight heparin (LMWH) can help protect against VTE in COVID-19 patients more significantly compared to aspirin or dypiridamole.