Cell death is a fundamental physiological process that all organisms undergo and is crucial for organ maintenance, autoimmunity, and embryonic development. Some of the different types of programmed cell death (PCD) include necroptosis, pyroptosis, apoptosis, and autophagy.
Recent studies have provided a better understanding of the mechanisms responsible for cell death and the crucial genes involved in these events. However, there remains a lack of information on the various types of cell death and their role in different illnesses.
In a recent study published in Cell Death Discovery, researchers elucidate the role of cell death in the pathogenesis of different diseases to ultimately identify novel targets for future drug discovery and diagnostic applications.
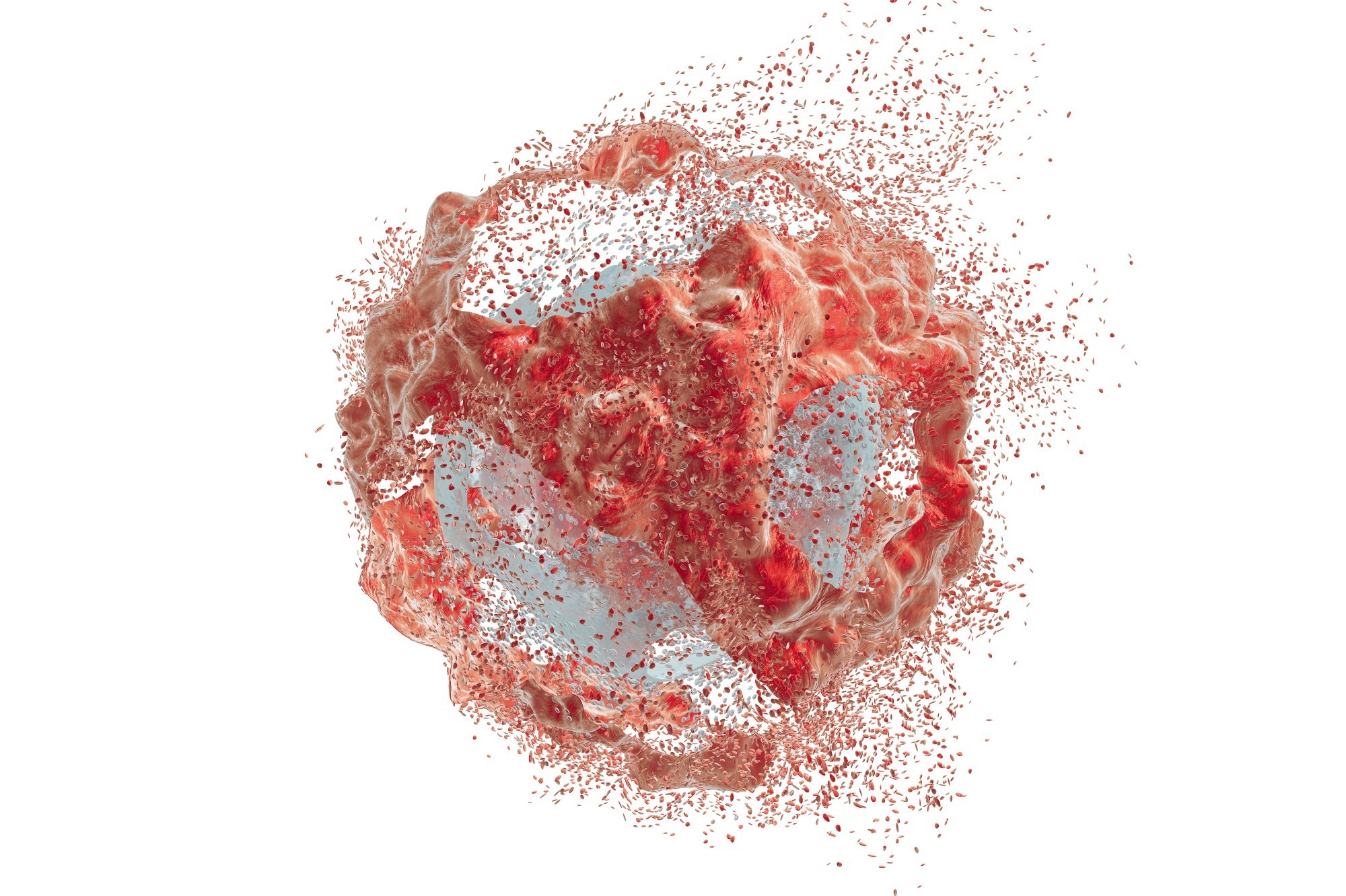 Study: Different types of cell death and their shift in shaping disease. Image Credit: Kateryna Kon / Shutterstock.com
Study: Different types of cell death and their shift in shaping disease. Image Credit: Kateryna Kon / Shutterstock.com
Different types of cell death
Apoptosis
Apoptosis is a process mediated by caspases that is essential for removing damaged or unwanted cells. During apoptosis, cell membranes shrink, chromatin agglutinates, apoptotic bodies form, and the cytoskeleton disintegrates.
Dependence and death receptors are crucial proteins involved in the endogenous pathway of apoptosis. After death, receptors bind to their ligands, stable trimer complexes, and formed and capable of recruiting proteins that eventually initiate the process of apoptosis.
The mitochondrial pathway in apoptosis is primarily mediated by the apoptotic inducible factor (AIF) protein, which can be transported from the mitochondria to the cytoplasm to cause DNA damage and cell death.
Pyroptosis
Pyroptosis comprises classical and non-classical pathways, in which classical pyroptosis begins with the increased expression of nuclear factor kappa-light-chain-enhancer of activated B cells (NF-kB). Thereafter, caspase-1 will cleave the N-terminal fragments of gasdermin D (GSDMD) to induce pyroptosis.
In the non-classical form of pyroptosis, caspases four, five, and 11 will cleave GSDMD to induce pyroptosis. These caspases can also cleave GSDMD, as well as interleukin 18 (IL-18) and IL-1β to induce pyroptosis and inflammation.
Necroptosis
As compared to necrosis, necroptosis is a caspase-independent process that occurs following the stimulation of tumor necrosis factor α (TNF-α). The combination of tumor necrosis factor receptor 1 (TNFR1) with TNF-α leads to the recruitment of various proteins that form complex I.
When caspase-8 is inhibited, the receptor-interacting protein kinase 1 (RIPK1) in complex I recruits RIPK3 and generates a necrosome. Necrosomes will ultimately be transferred from the cytoplasm to the cell membrane, wherein these organelles will form permeable pores within the membrane that ultimately results in cell death.
Autophagy
During autophagy, cytoplasmic organelles and proteins are engulfed, stored in vesicles, and eventually fused with lysosomes for degradation. Autophagy begins with autophagy induction, followed by autophagic membrane vesicle nucleation, autophagosome formation, and mature degradation.
Various signaling pathways are involved in autophagy, of which include phosphoinositide 3-kinase protein kinase B (PI3K-AkT), mitogen-activated protein kinase-extracellular signal-regulated kinase (MAPK-ERK), and adenosine monophosphate-activated protein kinase (AMPK) pathways.
The role of cell death conversions in disease development
GSDMs are key factors in the conversion of apoptosis to pyroptosis, whereas the conversion between apoptosis to necrosis is largely mitigated by ribosome-inactivating protein 1 (RIP1) and RIP3. RIP1 is responsible for the survival and death of a cell by activating the NF-kB signaling pathway. Increased expression of RIP3 reflects necrosis, whereas low RIP3 expression indicates apoptosis.
Notably, both RIP1 and RIP3 can combine to generate necrotic bodies, thereby leading to necroptosis. Rather than harm cells, this transition from apoptosis to necroptosis reduces the risk of resistance to chemotherapy drugs. Nevertheless, necroptosis pathway dysregulation has been associated with neurodegenerative, cardiovascular, and pulmonary disease.
The conversion between apoptosis and necroptosis has also been implicated in retinal diseases, as the loss of RIP3 expression prevents the formation of reactive oxygen species (ROS), thereby rescuing cone photoreceptor death. This observation led researchers to the hypothesis that inducing this cell death conversion through pharmaceutical agents could offer a therapeutic approach to treating retinal diseases.
Previous studies have shown that the upregulation of autophagy can reduce apoptosis in drug-resistant cancer cells. Thus, inducing the conversion between these two different types of cell death could improve the efficacy of many cancer drugs and reduce the risk of drug resistance and metastasis.
Comparatively, certain cancers like multiple myeloma (MM) exhibit increased levels of autophagy as compared to normal cells to support their survival in harsh conditions. Therefore, the inhibition of autophagy to increase apoptosis can lead to MM cell death.
Conclusions
The current study reports that the onset and progression of diseases are closely associated with the conversion of various types of cell death. These findings emphasize the significance of cell death as a target for different diseases; however, further research is needed to ensure that these strategies will not interfere with normal cellular processes and immune responses.