Introduction
SARS-CoV-2, which is the virus responsible for the ongoing pandemic of coronavirus disease 2019 (COVID-19), has infected over 424 million people worldwide and caused the deaths of over 5.88 million. As a result, there remains an urgent need for effective antiviral therapies. The SARS-CoV-2 spike protein is the primary target of most antivirals, neutralizing antibodies, and current COVID-19 vaccines.
The spike protein contains a receptor-binding domain (RBD) that binds to the host angiotensin-converting enzyme 2 (ACE2) receptor. Soon after binding to the ACE2 receptor, the RBD undergoes major conformational changes that allow this domain to transition from an open to a closed state. When the RBD is in an open conformation, it is accessible for binding between ACE2 and the receptor-binding motif (RBM).
At least one of the three RBDs on the spike homotrimer must be open to enable receptor binding, which primes the spike protein for further steps in infection. Each of the RBDs can transition from an open-to-closed state and vice versa, with the latter being associated with ACE2 priming. In fact, over half of spike proteins have one open RBD, a third have all three in the closed state, and one in seven have two open RBDs.
A clear understanding of how this transition occurs and how it can be controlled to prevent or treat infection would be very helpful. In one previous study, scientists demonstrated that the RBD has a free fatty acid (FFA)-binding pocket (FABP) that binds linoleic acid (LA) tightly and thereby becomes locked.
“Lined by hydrophobic residues, the RBD forms a kinked “greasy” tube that engulfs the hydrophobic free fatty acid (FFA) hydrocarbon chain of LA.”
The fatty acid is then anchored by residues in the adjacent RBD to form a polar lid to the pocket. This FABP is highly conserved among all three highly pathogenic coronaviruses, of which include SARS-CoV, SARS-CoV-2, and the Middle East Respiratory Syndrome Coronavirus (MERS-CoV).
The LA-induced locking shows that FFAs affect the conformational transition and, as a result, viral infectivity. Many different changes in the FFA profile have been reported in these infections. These important biomolecules are pro- and anti-inflammatory cytokine and signaling molecule precursors, and thus play a key role in the pathogenesis of COVID-19.
The current study reports the use of a bottom-up approach for assembling defined and low-complexity synthetic SARS-CoV-2-like particles called mini-virions (miniVs). These miniVs allowed the researchers to test spike binding at varying levels of FFA binding within the FABP in a low-biosafety level laboratory since the viral genome is absent. Furthermore, these SARS-CoV-2-like particles provided important information on how the spike protein regulates the immunogenicity and infectivity of this virus.
About the study
The researchers assembled the synthetic SARS-CoV-2 miniVs from reconstituted spike ectodomains using small unilamellar vesicles (SUVs). These particles show SARS-CoV-2-like cell attachment, with the characteristic biophysical features of these virions, which allowed the scientists to examine the effects of both particulate and multivalent binding.
With an average of 15 prefusion-stabilized spike particles per miniV, similar to that on the authentic virus, the scientists looked specifically at receptor binding apart from membrane fusion, since the cleavage site between the two subunits that triggers fusion was inactivated. Specific ACE2 binding was confirmed without significant attachment to the lipid membranes, like the actual virion.
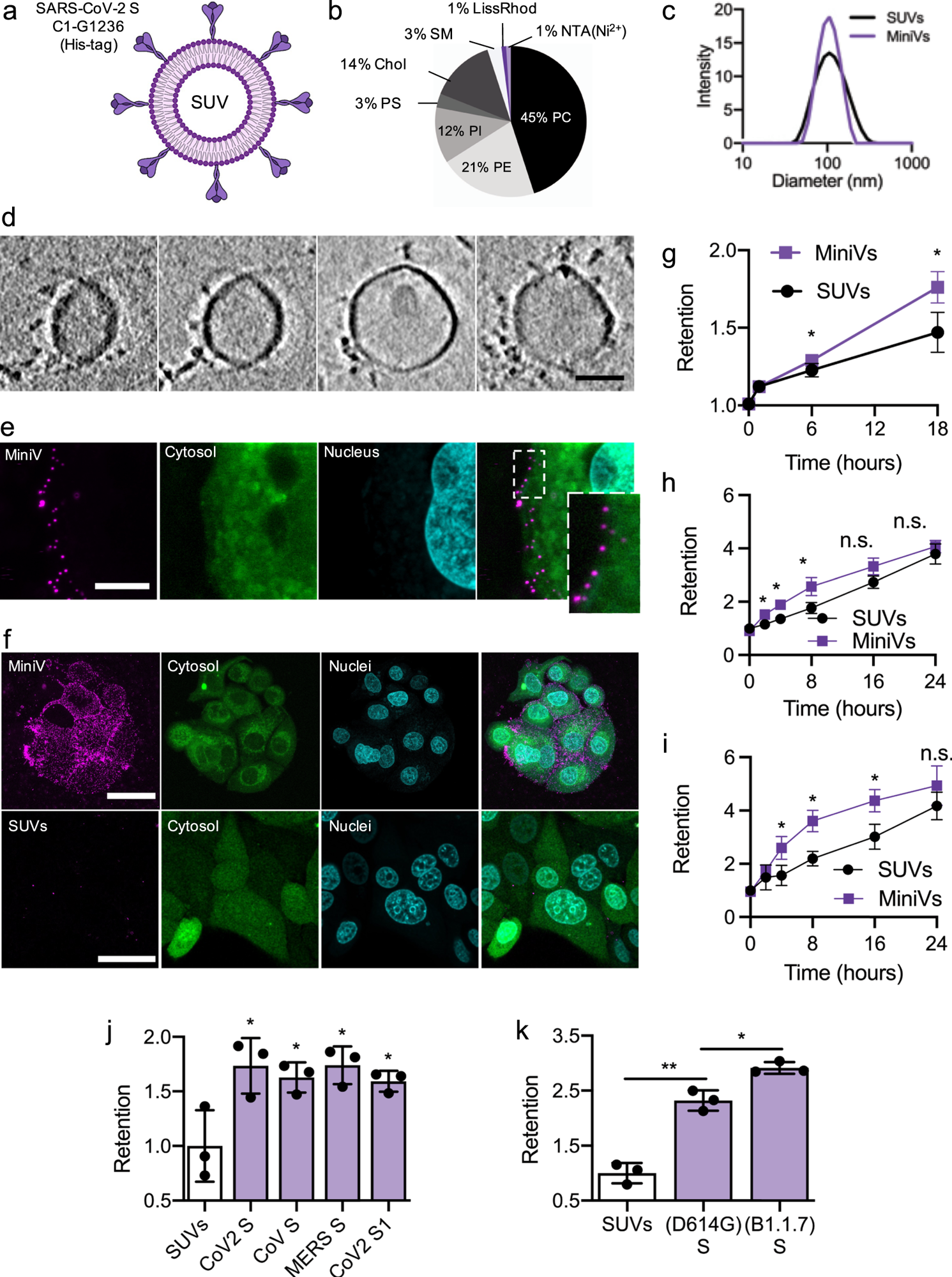
a Schematic illustration of MiniVs based on SUVs with SARS-CoV-2 S ectodomains, immobilized via their His-tag. b Lipid formulation of SUVs derived from the ERGIC with NTA-functionalized and fluorescent lipids. c MiniV and SUV size distribution analysis by dynamic light scattering. d Exemplary cryo-EM tomography slices of MiniVs with immobilized S on the membrane. Scale bar is 50 nm. e Representative confocal microscopy images, from two independent experiments, of MCF7 human epithelial cells incubated for 10 min with MiniVs, showing attachment of the MiniVs to the cells surface. Inset shows magnified area of attachment. Scale bar is 7 µm. f Maximal confocal microscopy z-projections of MCF7 human epithelial cells incubated for 18 h with MiniVs (top row) or with SUVs lacking S on the surface (bottom row). Scale bar is 40 µm. g–i Time-resolved retention assay of MiniVs and SUVs incubated with MCF7 (g), A549 (h), and HUVEC (i) cells. j SUV-normalized retention assay for MiniVs presenting different recombinant hCoV S variants incubated for 24 h with MCF7 cells. k Retention assay for MiniVs presenting SARS-CoV-2 D614G and B1.1.7 S variants incubated for 24 h with MCF7 human epithelial cells. Results in g–k are shown as mean ± SD from at least n = 3 biological replicates in each experimental condition, *p < 0.05, **p < 0.005, unpaired two-tailed t-test. Source data are provided as a Source Data file.
Compatible mimicry
Spike-associated increased binding to the ACE2-expressing cell, as well as with miniVs having only S1 subunit, and those bearing SARS-CoV or MERS-CoV spike ectodomains. The miniVs also blocked SARS-CoV-2 infection competitively, thereby showing their similarity of binding with the actual virions through cellular and receptor tropism. However, the SARS-CoV-2 Alpha variant-spike-bearing miniV showed enhanced binding due to higher receptor affinity.
“Taken together, MiniVs mimic the binding of natural SARS-CoV-2 viruses to target cells, faithfully simulating an early event in COVID-19.”
Thus, these particles provide a way to identify and study the effect of the FABP on the events surrounding virus-receptor attachment.
Among the four FFAs of palmitic acid (PA), oleic acid (OA), LA, and arachidonic acid (AA), all except PA reduced binding compared to the apo-spike protein. These three are polyunsaturated FFAs while PA is saturated. The unsaturated FFAs were found to pack into the kinked hydrophobic tubular FABP.
If the S1 domain was present without a trimeric structure, this effect was not seen because the anchoring effect on the FFAs was not possible without a second adjacent RBD in the trimeric protein. The FFAs affect spike-receptor binding directly, with no change in charge-based interactions with the miniV, despite the fact that the FFAs are negatively charged and are incorporated into the SUV membrane.
FABP required for virus-cell attachment
Spike cleavage mediated by transmembrane serine protease 2 (TMPRSS2) induces cell-virus membrane fusion for virus entry into the cell. Camostat mesylate, a TMPRSS2 inhibitor, prevents this event but does not have any obvious activity on the degree of retention of FFA-loaded miniVs. Thus, the FABP is required for the initial attachment of the virus to the cell and not for later events.
The novel K403R mutation in SARS-CoV-2, as compared to SARS-CoV, brought an RGD motif that consists of the tripeptide Arginine, Glycine, and Aspartate, into the RBD adjacent to the RBM. This may induce cell surface integrins to act as viral co-receptors and potentially mediates the increased infectivity of SARS-CoV-2.
In the current study, the position of the RGD motif in the LA-bound spike structure indicates that it can engage integrins for cell entry sequentially with the ACE2 receptor. The presence of unsaturated FFAs regulates the spike-integrin binding, likely by modulating the open-to-closed RBD transitions.
“Taken together, these results demonstrate that the FABP impacts S-mediated cell-binding, presumably via changes in the open-to-closed RBD equilibrium. It is also able to regulate RGD exposure and enhance integrin engagement by SARS-CoV-2 S.”
The researchers also explored the effectiveness of vitamin K and dexamethasone, two drugs that are important in the treatment of COVID-19. To this end, both drugs reduced spike-mediated miniV binding through the FABP at micromolar concentrations. Thus, the FABP appears to be a druggable region that regulates spike-receptor binding.
FABP regulates spike immunogenicity
The FABP is highly conserved among all SARS-CoV-2 variants and other highly pathogenic human coronaviruses, even though it does not enhance viral attachment to the host cell; rather, it may limit such binding. This indicates that its role is to facilitate the balance between virus-induced immunogenicity and infectivity.
The spike RBD is the immunodominant antigen of SARS-CoV-2, with over 90% of neutralizing antibodies and cells targeting this antigen. Using accessible surface area (ASA) measurements, the two antibodies of CR3022 and S2H14 were found to bind only to the RBD and be more accessible in the open conformation.
Conversely, the S2H13 epitope is slightly more accessible in the closed conformation. The key neutralizing sites appear more accessible in the open RBD state.
Unsaturated pro-inflammatory FFAs reduce neutralization efficiency against the FFA-loaded spike. It appears that binding of FFAs is a regulatory step in spike-neutralizing immunoglobulin G (IgG) activity, as it limits the exposure of neutralizing immunodominant sites (NIDS) when inflammatory cytokines are at their peak, thus providing a temporary escape.
Taken together, when FFAs are abundant, the FABP dynamically regulates spike immunogenicity by switching the RBD open-to-closed conformation, acting as a molecular switch.
“MiniV-based systematic assessment of S free fatty acid (FFA) binding reveals that FABP functions as an allosteric regulatory site enabling adaptation of SARS-CoV-2 immunogenicity to inflammation states via binding of pro-inflammatory FFAs. This is achieved by regulation of the S open-to-close equilibrium and the exposure of both, the receptor binding domain (RBD) and the SARS-CoV-2 RGD motif that is responsible for integrin co-receptor engagement.”
This mechanism may be successfully exploited for future COVID-19 treatment.