2. What should I know before I use Pradaxa?
Do not use if you have ever had an allergic reaction to dabigatran etexilate or any
of the ingredients listed at the end of the CMI.
Talk to your doctor if you have any other medical conditions, take any other medicines,
or are pregnant or plan to become pregnant or are breastfeeding.
3. What if I am taking other medicines?
4. How do I use Pradaxa?
Your doctor will tell you how many tablets you need to take each day.
Swallow the tablet(s) whole with a full glass of water.
5. What should I know while using Pradaxa?
|
Things you should do
|
Remind any doctor, dentist or pharmacist you visit that you are using Pradaxa.
If you are going to have any surgery or procedure, including dental surgery, tell
your surgeon, doctor or dentist that you are taking Pradaxa. Your doctor may decide
to temporarily stop your treatment with Pradaxa.
Tell your doctor or seek urgent medical attention if you fall or injure yourself during
treatment, especially if you hit your head, as you may be at increased risk of bleeding.
|
|
Things you should not do
|
Do not give Pradaxa to anyone else, even if they have the same condition as you.
Do not stop taking your medicine or lower the dosage without checking with your doctor
first.
|
|
Driving or using machines
|
Be careful before you drive or use any machines or tools until you know how Pradaxa
affects you.
Driving or operating machinery should be avoided for a period of time after orthopaedic
surgery.
|
|
Looking after your medicine
|
Keep your capsules in the blister pack until it is time to take them.
Keep Pradaxa in a cool dry place where the temperature stays below 30°C.
|
6. Are there any side effects?
Side effects may include bruising; nose bleeds; stomach ache; itchy skin, rash; diarrhoea;
indigestion; feeling sick; cough; painful, swollen joints; sore nasal passages and
throat; discomfort when swallowing; hair loss; frequent infections including symptoms
of fever, severe chills, sore throat or mouth ulcers. Serious side effects that require
urgent medical attention include long or excessive bleeding; exceptional weakness;
tiredness, headaches, dizziness and looking pale; chest pain or being short of breath;
swelling of hands, ankles and feet; red or dark brown urine; red or black bowel motions;
symptoms related to a condition called anticoagulant-related nephropathy such as blood
in urine, reduced urine output, swelling of legs, ankles and feet, increased time
for blood to clot, heavy bleeding.
Active ingredient:
dabigatran etexilate
Full Consumer Medicine Information (CMI)
This leaflet provides important information about using Pradaxa. You should also speak to your doctor or pharmacist if you would like further information
or if you have any concerns or questions about using Pradaxa.
Where to find information in this leaflet:
1. Why am I using Pradaxa?
Pradaxa contains the active ingredient dabigatran etexilate (as dabigatran etexilate
mesilate). After oral use, dabigatran etexilate is rapidly converted in the body to its active
form dabigatran. It belongs to a group of medicines called anticoagulants. Some people
refer to anticoagulant medicines as "blood thinners". Dabigatran works by inhibiting
a specific protein in the blood, called thrombin. Thrombin contributes to the formation
of blood clots. Dabigatran prevents the formation of blood clots.
Pradaxa is used to:
prevent the formation of blood clots in the veins after knee or hip replacement surgery
in adults
reduce the risk of brain (stroke) and/or other body vessel obstruction by blood clot
formation in adults with an abnormal heart beat rhythm called non-valvular atrial
fibrillation
treat blood clots in the veins of your legs and lungs and to prevent blood clots from
re-occurring in the veins of your legs and/or lungs.
2. What should I know before I use Pradaxa?
Warnings
Do not use Pradaxa if:
you are allergic to dabigatran etexilate, or any of the ingredients listed at the
end of this leaflet.
Always check the ingredients to make sure you can use this medicine.
you are currently bleeding
you have severely reduced kidney function (your doctor will know how to determine
your kidney function)
you have an increased tendency of bleeding complications (this may be inherited, of
unknown cause or due to other medicines)
you have a medical condition which increases your risk of serious bleeding, such as
recent brain or spinal injury, and cancer
you have active stomach ulcers or have experienced stomach bleeding in the past year,
unless the cause has been permanently eliminated, e.g. by surgery
you have a history of bleeding in the head, eyes, spine, abdomen and joints
you have an indwelling spinal or epidural catheter, and during the first two hours
after their removal (your doctor will know about the kind of catheters and precautionary
measures)
you have liver problems or liver disease
you have a prosthetic heart valve.
Do not use Pradaxa if you are taking the following medicines:
oral ketoconazole or itraconazole, medicines used to treat fungal infections
dronedarone, a medicine used to treat abnormal heart beat
ciclosporin or tacrolimus, medicines used to prevent organ rejection after transplantation
glecaprevir/pibrentasvir, a combination medicine used to treat hepatitis C infection
medicines to prevent blood clotting (e.g. warfarin, rivaroxaban, apixaban or heparin),
except when changing anticoagulant treatment, while having a venous or arterial line
and you get heparin through this line to keep it open or while your heart beat is
being restored to normal by a procedure called catheter ablation for atrial fibrillation
verapamil, a calcium channel blocker used to treat high blood pressure and angina.
Do not start Pradaxa and verapamil treatment at the same time. Do not start verapamil
if you are currently taking Pradaxa and have just undergone major orthopaedic surgery.
If you are not sure whether you should start taking this medicine, talk to your doctor.
Check with your doctor if you:
take any medicines for any other condition
have any other medical conditions
have allergies to any other medicines, foods, preservatives or dyes
have had a heart attack or if you have been diagnosed with conditions that increase
the risk to develop a heart attack
have reduced liver function, life-threatening liver disease or increased liver enzymes.
have an increased risk of bleeding, as could be the case in the following situations:
if you are older than 75 years, your doctor may prescribe a lower dose of Pradaxa
if you know you have reduced kidney function, or you are suffering from dehydration
(symptoms include feeling thirsty and passing reduced amounts of dark-coloured urine)
if you have been recently bleeding
if you have any problems with your blood
if you have had a recent tissue sampling (biopsy)
if you have cancer
if you have had a serious injury (e.g. a bone fracture, head injury or any injury
requiring treatment)
if you are suffering from an inflammation of the food pipe (oesophagus) or stomach
if you have problems with reflux of gastric juice into the food pipe (oesophagus)
if you are receiving medicines which could increase the risk of bleeding, such as
clopidogrel and warfarin
if you are taking anti-inflammatory medicines such as diclofenac
if you are suffering from an infection of the heart (bacterial endocarditis).
know that you have a disease called antiphospholipid syndrome (a disorder of the immune
system that causes an increased risk of blood clots).
If you have not told your doctor about any of the above, tell them before you use
Pradaxa.
During treatment, you may be at risk of developing certain side effects. It is important
you understand these risks and how to monitor for them. See additional information
under Section
6. Are there any side effects?
Pregnancy and breastfeeding
Do not take Pradaxa if you are pregnant.
It may affect your developing baby if you take it during pregnancy.
Check with your doctor if you are pregnant or intend to become pregnant.
Do not breastfeed if you are taking Pradaxa.
The active ingredient in Pradaxa passes into breast milk.
Talk to your doctor if you are breastfeeding or intend to breastfeed.
Use in Children
Do not give this medicine to a child or adolescent under 18 years old.
3. What if I am taking other medicines?
Tell your doctor or pharmacist if you are taking any other medicines, including any
medicines, vitamins or supplements that you buy without a prescription from your pharmacy,
supermarket or health food shop.
Some medicines may interfere with Pradaxa and affect how it works. These include:
aspirin, salicylates or other NSAID (anti-inflammatory) medicines
medicines used to thin your blood (such as warfarin, unfractionated heparins, heparin
derivatives (fondaparinux and desirudin), low molecular weight heparins (enoxaparin),
clopidogrel, tirofiban, bivalirudin, prasugrel, ticagrelor, eptifibatide, ticlopidine,
dextran, sulfinpyrazone, rivaroxaban and apixaban)
amiodarone, dronedarone, medicines used to treat irregular heartbeats
verapamil, a calcium channel blocker used to treat high blood pressure and angina
quinidine, a medicine used to treat malaria and irregular heartbeats
clarithromycin or rifampicin, medicines used to treat infections
lopinavir, nelfinavir, ritonavir, tipranavir or saquinavir, medicines used to treat
HIV infections
ciclosporin or tacrolimus, medicines used to help the body's immune system
glecaprevir/pibrentasvir, a combination medicine used to treat hepatitis C infection
selective serotonin re-uptake inhibitors (SSRI) (e.g. citalopram, escitalopram, fluoxetine),
selective serotonin norepinephrine re-uptake inhibitors (SNRI) (e.g. duloxetine, venlafaxine,
desvenlafaxine), medicines used to treat mood disorders
herbal medicines derived from St John's wort (Hypericum perforatum)
carbamazepine, a medicine used to treat fits or convulsions
medicines used to treat reflux and stomach ulcers (such as pantoprazole and ranitidine).
These medicines may be affected by Pradaxa or may affect how well it works. You may
need different amounts of your medicines, change the timing of your medicine-taking
routine or take different medicines. Your doctor or pharmacist will advise you.
Check with your doctor or pharmacist if you are not sure about what medicines, vitamins
or supplements you are taking and if these affect Pradaxa.
4. How do I use Pradaxa?
Follow the instructions given to you by your doctor or pharmacist carefully. They may differ from the information contained in this leaflet.
If you do not understand the instructions on the box, ask your doctor or pharmacist
for help.
How much to take
After knee and hip replacement surgery
The recommended dose of Pradaxa is 220 mg (2 capsules of 110 mg) taken as a single
dose once daily.
Patients with moderately reduced kidney function (e.g. over 75 years) or patients
taking certain medicines may have an increased risk of bleeding. The doctor may prescribe
the lower dose of 150 mg once daily, taken as 2 capsules of Pradaxa 75 mg.
Treatment with Pradaxa should be started within 1 - 4 hours of completed surgery,
using a single capsule of 110 mg and continuing with 2 capsules of 110 mg once daily
for a total of 10 days (after knee replacement surgery) or for a total of 28 - 35
days (after hip replacement surgery).
If, within 4 hours after surgery, post-operative bleedings can still be observed,
initiation of treatment should be delayed. If treatment is not started on the day
of surgery then treatment should be initiated with 2 capsules of 110 mg once daily.
For stroke prevention in patients with atrial fibrillation
The recommended dose of Pradaxa is 300 mg taken as 1 capsule of 150 mg in the morning
and 1 capsule of 150 mg in the evening.
Patients over 75 years should take a lower dose of 220 mg, taken as 1 capsule of 110
mg in the morning and 1 capsule of 110 mg in the evening.
Patients with an increased risk of major bleeding (as determined by your doctor) should
take a lower dose of 220 mg, taken as 1 capsule of 110 mg in the morning and 1 capsule
of 110 mg in the evening.
For the treatment of blood clots and prevention of blood clots re-occurring in the
veins of your legs and/or lungs
The recommended dose of Pradaxa is 300 mg taken as 1 capsule of 150 mg twice a day
following treatment with an injectable blood thinner for at least 5 days. To prevent
blood clots re-occurring, continue on 1 capsule of 150 mg twice a day.
Patients over 75 years should take a lower dose of 220 mg, taken as 1 capsule of 110
mg in the morning and 1 capsule of 110 mg in the evening. To prevent blood clots re-occurring,
continue on 1 capsule of 110 mg twice a day.
Patients with an increased risk of major bleeding (as determined by your doctor) should
take a lower dose of 220 mg, taken as 1 capsule of 110 mg in the morning and 1 capsule
of 110 mg in the evening. To prevent blood clots re-occurring, continue on 1 capsule
of 110 mg twice a day.
Your doctor will decide how long you need to be on this treatment for.
When to take Pradaxa
Take Pradaxa at about the same time each day.
Taking your capsules at the same time each day will have the best effect. It will
also help you remember when to take it.
How long to take Pradaxa
Continue taking your medicine for as long as your doctor tells you.
Pradaxa will continue to be prescribed while there is a risk of excessive clotting.
After knee replacement surgery:
This will usually be for a period of 10 days.
After hip replacement surgery:
This will usually be for a period of 28 - 35 days.
It is important to keep taking your medicine even if you feel well.
If you stop using Pradaxa before your doctor tells you to stop, you are at risk of
developing a blood clot in a vein of your leg which can move to the lungs and be life-threatening.
Tell your doctor immediately or go to Emergency at your nearest hospital if you notice
swelling of the leg or cough and shortness of breath.
These could be signs of a blood clot.
Tell your doctor if you intend stopping treatment earlier.
For stroke prevention in patients with atrial fibrillation:
It is important to keep taking your medicine even if you feel well.
If you stop using Pradaxa before your doctor tells you to stop, you are at risk of
developing a blood clot. This can lead to serious health problems such as strokes.
For treatment and prevention of blood clots re-occurring in the veins of your legs
and lungs:
It is important to keep taking your medicine even if you feel well.
If you stop using Pradaxa before your doctor tells you to stop, you are at risk of
developing a blood clot. This can lead to serious health problems if those clots stop
blood flowing normally.
How to take Pradaxa
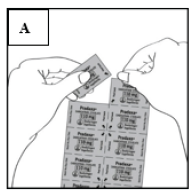
Removing Pradaxa capsules from the blister pack
Prior to removing a capsule from the blister card, separate one blister segment by
tearing along the perforations (Figure A).
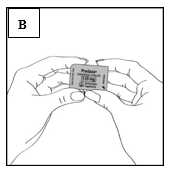
Once you have separated an individual blister segment, locate the tab marked with
the arrow (Figure B).
Immediately before you are ready to take your dose of Pradaxa, peel back the foil
using the tab marked with the arrow until the capsule is fully visible (Figure C).
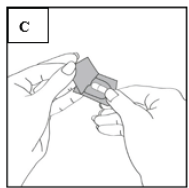
Turn the blister segment upside down and tip the capsule out, tapping the back of
the blister segment, if necessary.
Do not try to push the capsule through an unopened blister segment.
Do not cut the foil or use sharp instruments to remove the capsule from the blister.
Capsules should always be stored in the sealed blister segments and only removed immediately
before use. The capsule should be taken immediately after the foil over an individual
blister segment is opened, or its effectiveness may be reduced.
If additional capsules are inadvertently exposed to air, they should not be used and
should be discarded.
Capsules should not be removed from the blister pack and repackaged in dose administration
aids such as dosette boxes, tablet organisers or weekly medication packs.
Swallow the capsules whole with a full glass of water.
It does not matter if you take this medicine with or without food.
Do not chew or open the capsule. Do not sprinkle the pellets on food or mix with liquids.
This may cause an overdose of Pradaxa and increase the risk of bleeding.
If you forget to use Pradaxa
After knee and hip replacement surgery continue with your remaining daily doses of
Pradaxa at the same time of the next day. Do not take a double dose to make up for
the dose you missed.
For stroke prevention in patients with atrial fibrillation a forgotten dose of Pradaxa
can still be taken up to 6 hours prior to the next dose. A missed dose should be omitted
if the remaining time is less than 6 hours prior to the next dose. Do not take a double
dose to make up for the dose you missed.
For the treatment and prevention of blood clots re-occurring in the veins of your
legs and lungs a forgotten dose of Pradaxa can still be taken up to 6 hours prior
to the next dose. A missed dose should be omitted if the remaining time is less than
6 hours prior to the next dose. Do not take a double dose to make up for the dose
you missed.
If you are not sure what to do, ask your doctor or pharmacist.
If you have trouble remembering when to take your medicine, ask your pharmacist for
hints.
If you use too much Pradaxa
If you think that you have used too much Pradaxa, you may need urgent medical attention.
You should immediately:
phone the Poisons Information Centre
(by calling
13 11 26), or
contact your doctor, or
go to the Emergency Department at your nearest hospital.
You should do this even if there are no signs of discomfort or poisoning.
If you take too much Pradaxa you may have bleeding. Blood may be seen in stools or
urine. Abnormal bruising may also be experienced.
5. What should I know while using Pradaxa?
Things you should do
Remind any doctor, dentist or pharmacist you visit that you are using Pradaxa.
Tell your doctor if, for any reason, you have not used Pradaxa exactly as prescribed.
Otherwise, your doctor may think that it was not effective and change your treatment
unnecessarily.
If you become pregnant while using Pradaxa, tell your doctor immediately.
If you are going to have any surgery or procedure, including dental surgery, tell
your surgeon, doctor or dentist that you are taking Pradaxa.
Your doctor may decide to temporarily stop your treatment with Pradaxa.
Tell your doctor if you fall or injure yourself during treatment, especially if you
hit your head, please seek urgent medical attention.
You may need to be checked by a doctor, as you may be at increased risk of bleeding.
Things you should not do
Do not give Pradaxa to anyone else, even if they have the same condition as you.
Do not stop taking your medicine or lower the dosage without checking with your doctor.
Driving or using machines
Be careful before you drive or use any machines or tools until you know how Pradaxa
affects you.
Driving or operating machinery should be avoided for a period of time after orthopaedic
surgery.
Looking after your medicine
Keep your capsules in their blister pack until it is time to take them. If you take
the capsules out of the blister pack they may not keep well.
Keep Pradaxa in a cool dry place where the temperature stays below 30°C.
Follow the instructions in the carton on how to take care of your medicine properly.
Store it in a cool dry place away from moisture, heat or sunlight; for example, do
not store it:
in the bathroom or near a sink, or
in the car or on window sills.
Keep it where young children cannot reach it.
A locked cupboard at least one-and-a-half metres above the ground is a good place
to store medicines.
Getting rid of any unwanted medicine
If you no longer need to use this medicine or it is out of date, take it to any pharmacy
for safe disposal.
Do not use this medicine after the expiry date.
6. Are there any side effects?
All medicines can have side effects. If you do experience any side effects, most of
them are minor and temporary. However, some side effects may need medical attention.
See the information below and, if you need to, ask your doctor or pharmacist if you
have any further questions about side effects.
Side effects
|
Side effects
|
What to do
|
|
Bleeding-related:
nose bleeds
Gastrointestinal-related:
stomach ache
diarrhoea
indigestion
feeling sick
discomfort when swallowing
Skin and hair-related:
bruising
itchy skin, rash
hair loss
Infection-related:
frequent infections including fever, severe chills, sore throat or mouth ulcers (signs
of lack of white blood cells)
sore nasal passages and throat
Lungs-related:
cough
Musculoskeletal:
painful, swollen joints
|
Speak to your doctor if you have any of these side effects and they worry you.
|
Serious side effects
|
Serious side effects
|
What to do
|
|
Bleeding-related
long or excessive bleeding
Kidney-related:
red or dark brown urine
swelling of hands, ankles and feet
Gastrointestinal-related:
red or black bowel motions
Nervous system-related:
exceptional weakness
Respiratory-related:
chest pain or being short of breath
Symptoms related to an allergic reaction:
rash, itching or gives on the skin
swelling of the face, lips, tongue or other parts of the body
shortness of breath, wheezing or troubled breathing
Symptoms related to anaemia
tiredness
headaches
dizziness
looking pale
Symptoms related to a condition called anticoagulation-related nephropathy
blood in urine
reduced urine output
swelling of the legs, ankles and feet
increased time for blood to clot (high INR test values)
heavy bleeding.
|
Call your doctor straight away, or go straight to the Emergency Department at your
nearest hospital if you notice any of these serious side effects.
|
Tell your doctor or pharmacist if you notice anything else that may be making you
feel unwell.
Other side effects not listed here may occur in some people.
Reporting side effects
After you have received medical advice for any side effects you experience, you can
report side effects to the Therapeutic Goods Administration online at
www.tga.gov.au/reporting-problems . By reporting side effects, you can help provide more information on the safety of
this medicine.
Always make sure you speak to your doctor or pharmacist before you decide to stop
taking any of your medicines.
7. Product details
This medicine is only available with a doctor's prescription.
What Pradaxa contains
|
Active ingredient
(main ingredient)
|
Pradaxa 75 mg - 75 mg dabigatran etexilate given as 86.48 mg dabigatran etexilate mesilate per
capsule.
Pradaxa 110 mg - 110 mg dabigatran etexilate given as 126.83 mg dabigatran etexilate mesilate per
capsule.
Pradaxa 150 mg - 150 mg dabigatran etexilate given as 172.95 mg dabigatran etexilate mesilate per
capsule.
|
|
Other ingredients
(inactive ingredients)
|
Capsule fill
acacia
dimeticone 350
hyprolose
hypromellose
purified talc
tartaric acid
Capsule shell
carrageenan
potassium chloride
titanium dioxide
indigo carmine CI73015 (110 mg and 150 mg capsules only)
hypromellose
purified water
Black printing ink
TekPrint SW-9008 Black Ink.
|
Do not take this medicine if you are allergic to any of these ingredients.
Pradaxa does not contain gluten, sucrose or tartrazine.
What Pradaxa looks like
Pradaxa is the brand name of your medicine.
Pradaxa is available in three strengths of capsules:
Pradaxa 75 mg capsules (AUST R 137832): white-coloured, opaque cap and body, imprinted
with a R75 code on one side and company logo on the other
Pradaxa 110 mg capsules (AUST R 138402): light blue-coloured, opaque cap and body,
imprinted with a R110 code on one side and company logo on the other
Pradaxa 150 mg capsules (AUST R 168211): light blue-coloured, opaque cap with a white-coloured,
opaque body imprinted with a R150 code on one side and company logo on the other.
Pradaxa 75 mg, 110 mg and 150 mg are available in blister packs of 10* and 60 capsules.
Pradaxa 75 mg and 110 mg are also available in blister packs of 30** capsules.
* Only for the Pradaxa 110 mg
** Not distributed in Australia.
Who distributes Pradaxa
Pradaxa is supplied in Australia by:
Boehringer Ingelheim Pty Limited
ABN 52 000 452 308
Sydney, Australia
This leaflet was prepared in July 2025.
® Pradaxa is a registered trademark of Boehringer Ingelheim.
© Boehringer Ingelheim Pty Limited 2025