Pelvic inflammatory disease (PID) is a consequence of the infection of the upper genital tract in women, resulting in a plethora of pathological pelvic findings (ranging from mild endometritis to peritonitis). Putative microorganisms are either sexually-transmitted pathogens (most notably Chlamydia trachomatis and Neisseria gonorrhoeae, but also Mycoplasma genitalium) or endogenously present vaginal microorganisms that ascend from the lower genital tract via the cervix into the pelvic region.
Appropriately diagnosing PID is often cumbersome and quite challenging, as the infectious process may be localized or widespread. Moreover, the symptoms and signs of the disease can range from none or subtle to severe, microbiologic assessment is usually not readily available, while more accurate and specific diagnostic modalities are invasive and costly.
The recommendation from the US Centers for Disease Control (CDC) is a low threshold for diagnosis of PID, since the concern for the potential damage of the female reproductive health caused by missed cases surpasses the more comprehensive approach. Due to this, only after the presence of a minimum number of clinical criteria has been confirmed (such as abdominal pain, cervical motion and adnexal tenderness) will additional diagnosis to enhance the specificity be pursued.
Laboratory testing
Since PID is predominantly a clinical diagnosis, extensive diagnostic procedures are not always necessary, although they can aid in establishing the correct diagnosis or defining its severity. For example, the absence of polymorphonuclear leukocytes when observing saline wet mount prepared from vaginal secretions can exclude histologic endometritis in more than 90 percent of cases.
Cervical and high vaginal swab cultures for both aerobic and anaerobic organisms are usually pursued, whereas urethral swab culture may be done if gonorrhea is suspected as the causative agent. Serological microfluorescence test for the detection of IgG and IgM antibodies is useful, but the current diagnostic recommendations include the use of molecular methods (such as polymerase chain reaction) to maximize the diagnostic yield.
Invasive examinations
Laparoscopically confirmed visual findings of edema and erythema of the fallopian tubes, clubbing of the fimbriae or the presence of tubo-ovarian abscess are considered the gold standard for diagnosing PID. Nevertheless, since laparoscopy is an invasive procedure that is not routinely performed on women with suspected disease, a majority of cases are diagnosed based on clinical presentation.
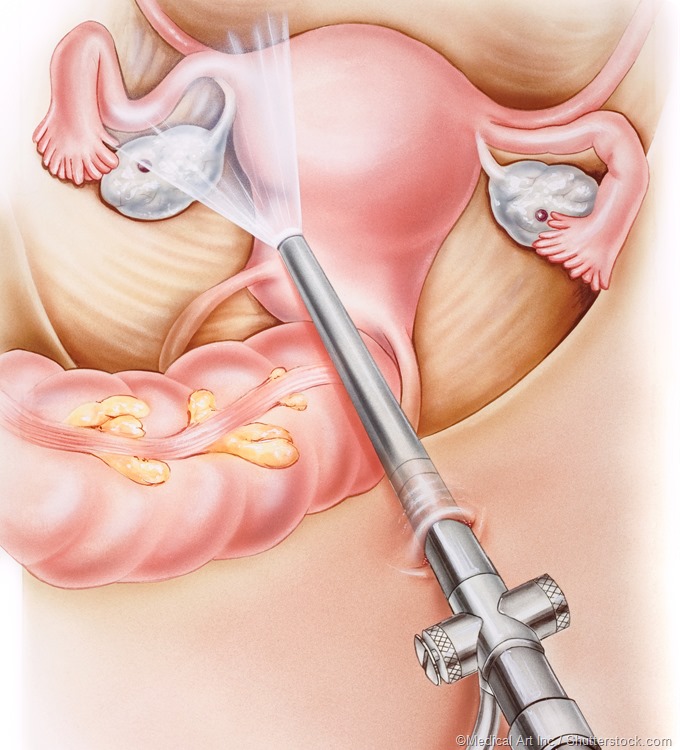
Laparoscopy illustration showing the ovaries, fallopian tubes, uterus, and colon.
Endometrial biopsy that can be used to demonstrate endometrial inflammation shows good sensitivity and specificity, thus it has been suggested as a less invasive alternative to laparoscopy for confirming a clinical diagnosis of acute PID. Finding neutrophils and plasma cells located in the endometrium is highly indicative and, therefore, used to diagnose PID.
Imaging studies
Ultrasonography (or ultrasound) is a widely available and helpful noninvasive tool that can also be used to aid in the diagnosis of PID. If thickened fallopian tubes filled with fluid are observed, ultrasound evaluation can be considered 85 percent sensitive and 100 percent specific for establishing endometritis in women with clinically-diagnosed PID.

Computed tomography (CT) is usually reserved for evaluating the extent of PID within the abdominal cavity. In early PID the most common findings are cervicitis, salpingitis, oophoritis, thickened uterosacral ligaments, and fluid in the fallopian tubes and pelvis. Of course, a drawback of employing this technology is exposing the patient to ionizing radiation, which is not advised in young women.
Magnetic resonance imaging (MRI) is highly sensitive and specific in identifying thickened tubes filled with fluid, fluid in the pelvis, pyosalpinx, and tubo-ovarian abscesses. For these reasons, it has been proposed as another diagnostic modality for PID. Nevertheless, it is very expensive for the patient and not within reach for women seeking outpatient assessment for possible PID.
Further Reading
Last Updated: Feb 27, 2019