Breast cancer is the leading cause of cancer-related death among the female population globally, despite the ever-growing technology of early detection.
In this interview, Dr. Tone Frost Bathen, Head Professor at MR Cancer Group explains how using NMR based metabolomics can help with the identification of Breast Cancer.
Please tell us about your area of focus.
My research group, the MR Cancer Group, is situated at the Norwegian University of Science and Technology in Trondheim. We are an interdisciplinary research group, and our primary focus is cancer research. Metabolomics has since the early 2000s been one of our main methodologies. Importantly, this is combined with other molecular analysis and imaging. We use magnetic resonance technology for improved cancer treatment and patient care, but we are also involved in other biomedical applications.
Can you discuss your imaging approaches to cancer research?
We maintain several biobanks with tissue and biofluids from cancer patients, have access to relevant animal models of cancer and take part in clinical imaging trials. The equipment ranges from spectrometers dedicated to metabolomics research, animal scanners, and high-field clinical scanners. Magnetic resonance has ample opportunities to provide relevant information about the acquired capabilities for cancer. Dynamic contrast-enhanced magnetic resonance imaging (MRI) enables visualization of tumors. We can do diffusion MRI, which helps us gain insight into the cellularity of tissue under investigation. We can obtain molecular information from hybrid imaging, and we can study metabolism using in vivo or ex vivo magnetic resonance spectroscopy.
Image Credit:Shutterstock/jovan vitanovski
Can you discuss metabolomics and how you use it in your research?
Metabolomics is a branch of omics methods, involving high-level identification and quantification of metabolites. In biofluid analysis, for example, sera are mixed with a buffer, transferred to NMR tubes, and then ready for analysis by a spectrometer. For biofluids, we have implemented in vitro diagnostics protocols. This standardized analytical scheme enables detection and qualification of protein subclasses and small molecular metabolites.
High-resolution spectra are obtained through magic angle spinning and NMR spectroscopy using a special probe. This situation mimics the molecular rotation of the liquid and results in spectra with comparable resolution to liquids. Several metabolites can be quantified. I must admit, that in our labs, at least the analysis of intact tissue still relies generally on manual work. However, we have standardized acquisition protocols, and now use an acquisition scheme which is similar to what is used per serum sample. Today I will talk about serum and tissue analysis.
So, metabolomics can be applied for applications along the entire timeline of cancer and potentially inform the diagnosis and treatment monitoring by detection of prognostic and predictive biomarkers. Metabolomics can also aid in the mechanistic understanding of the molecular changes occurring in cancer progression and treatment.
ImageCredit:Shutterstock/CI Photos
How do nuclear magnetic resonance (NMR) techniques fit in with your practice?
It is important to remember that nuclear magnetic resonance (NMR) is another useful tool for measurement. The spectrum obtained is an average across the whole sample. The total sample composition, including dermal cells in a complete microenvironment, will contribute to the spectral fingerprint. As metabolite concentrations in serum are regulated by numerous homeostatic mechanisms in the body, it may be challenging to relate metabolic profiles in serum directly to the cancer cell metabolism. NMR also has relatively low sensitivity, and potential metabolites excreted by a tumor may not be detectable.
In a recent study, we measured metabolites in tumor tissue and serum from the same breast cancer patient. There were quite strong correlations between metabolites measured within serum and within the tissue, but the correlations between metabolites observed in tissue and serum were low. It is therefore important to remember that what we observe by measuring serum metabolites in cancer patients is more related to tumor-host interaction. Also, the serum metabolites in a cancer patient will be influenced by several other variables, such as diet, medication, and smoking, but also factors such as genetics, body composition, physical activity, microbiome, endocrine response, mental stress, inflammation, and circadian rhythms.
Tell us about your experience using metabolomics with breast cancer?
The presence of the human epidermal growth factor receptor 2 (HER2), promotes the growth of tumor cells. However, because targeted treatments are now available, prognoses now are actually quite good, this even includes HER2-positive patients. Triple-negative breast cancer is a subgroup where the tumor is negative for ER, TTR, and HER2-positive. This is a challenging subgroup with a relatively poor prognosis. Currently, no targeted treatment is available for this patient group, and treatment is mainly restricted to chemotherapy.
Before moving into the metabolic characteristics of cancer, it is important to know that we can observe differences between tumor tissue and normal adjuvant tissue. This work was carried out using samples from our regional biobank. The tissue samples were analyzed using magic angle spinning. We established a PLS-DA model to differentiate between tumor and normal tissue. The prediction accuracy was about 90%.
The subgroup of estrogen receptor-positive breast cancer patients is associated with a relatively good prognosis. We wanted to investigate the metabolic characteristics related to this. ER-positive and ER-negative breast cancer patients can be differentiated with an accuracy of 88%. In the low-risk profile, we saw that ER-negative patients had higher levels of glycine, choline,, and alanine. We have also investigated the characteristics of triple-negative breast cancer, and this study showed increased levels of choline, which are probably related to the increased proliferation seen in triple-negative breast cancer.
In our study, the genetic subtype based on transcriptome analysis was also the same tissue. And interestingly, there was no accumulation of a genetic subtype within the metabolic clusters. The genetic subtypes are evenly distributed. The metabolic clusters demonstrated distinct characteristics, such as elevated choline metabolism, elevated lactate, and reduced choline metabolism. These are patterns that could be exploited for treatment, such as utilizing metabolic inhibitors to target choline metabolism or stimulating lactate conversion through lactate dehydrogenase. The last cluster potentially points towards a less aggressive subgroup where there's high glucose to lactate ratio. But the validation using long-term follow up for the patient needs to be performed to confirm this.
Overall, ER-positive patients are considered to have a relatively good prognosis, but some patients still relapse. Using principal components analysis, or the spectra from the ER, we observed samples from patients that passed away within 5 years after diagnosis. The variables defined in this population were glycine and lactate. Lactate is related to the Warburg Effect, while glycine, again probably reflects rapidly proliferating cells using glycine to a nucleotide.
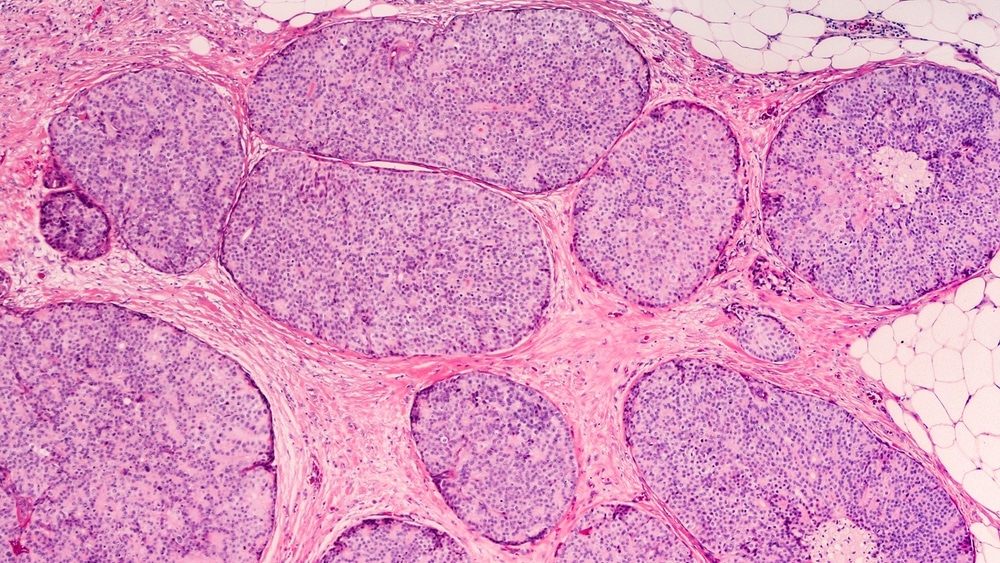
Image Credit:Shutterstock/David A Litman
Please tell us about your study using metabolic profiling of breast cancer treated with chemotherapy?
The samples in the study were subjected to a global metabolic profiling using a combination of NMR and mass spectrometry. Looking into the changes in small molecular metabolites measured by NMR and mass spectrometry, we found a significant change in the metabolic profile from baseline to six months, in patients receiving chemotherapy. The findings reflect the changes related to inflammation, immune response, and increased risk of cardiovascular disease. Surprisingly, there were also changes in patients that did not receive chemotherapy. It is possible that radiation therapy may have had an effect.
Looking into the results from the lipoprotein subclass analysis in the same pilot cohort, we also detected significant responses to chemotherapy. All the LDL and small LDL subclasses increased after 6 months, while HDL decreased. In addition, significant triglyceride enrichment was observed in HDL and LDL subclasses. These changes are descriptive of an atherogenic inflammatory lipid profile and provides a much more detailed picture of the lipoprotein metabolism when compared to the standard lab measurements, where the only detected changes included an overall increase of triglycerides and a decrease in HDL cholesterol.
In a patient that did not receive chemotherapy after surgery, we observed that the LDL subclasses were less increased, there was triglyceride enrichment, and LDL subclasses decreased. For this group, the standard lab measurements showed no changes, but overall, the changes that we observed here persisted through 12 months. This was reflected by an atherogenic inflammatory lipid profile showing potential side effects from the chemotherapy that breast cancer patients received.
This is a non-destructive technique. How does it compare with those using destructive MS techniques?
If we compare to mass spectrometry, I would say that the main advantage of NMR is that you do not need to treat the sample in a specific way. You just cut it, add some buffer, and then it is ready for the analysis. However, NMR spectroscopy is much less sensitive for metabolite detection compared with mass spectrometry. However, NMR is by nature a more quantitative method and I would say also quite reproducible. For mass spectrometry, there are now approaches where you can use the intact tissue sample for mass spectrometry imaging, and you can also use fresh frozen tissue for that. But the sample will be partially destroyed by the lasers applied during mass spectrometry imaging.
What are the pros and cons of NMR-based metabolomics compared with MS-based methods?
I would say they are complementary techniques, but the major pro for NMR is that you have no lasered sample preparation before the analysis, regardless as to whether it is a tissue sample or a serum or urine sample. You add a buffer and the sample is ready to be analyzed. But for mass spectrometry, you will often need to extract the sample.
How important is metabolomics and NMR for the future of science?
We need to open science in order to compare various strategies and to validate our findings in several cohorts. Most published studies so far are small, and they also need larger cohort studies for validation. Importantly, metabolomics can be used across several disciplinary fields. Close interaction between technologists and clinicians is necessary to maximize the potential value of the analysis. In summary, NMR based metabolomics is a versatile tool in cancer research.
Numerous studies show promising results across the cancer timeline; However, clinical implementation is still low. That is not to say it is non-existent. Standardization, validation, and open science are important aspects to translate the methodology to clinical application. To this end, technologies in the clinic need to work in concert to move the field forward.
About Dr. Tone Frost Bathen
As head of the MR Cancer Group, Bathen’s main research interests are focused on personalized medicine and studies of functional and metabolic properties of cancer, using magnetic resonance imaging (MRI) and spectroscopy (MRS). By developing, optimizing, and applying advanced MR (in combination with other molecular methods) to characterize cancer, the group’s goal is to establish better diagnostic tools for the stratification of patients to treatment and treatment monitoring. Current research activities mainly focus on breast and prostate cancer, enabled by a close collaboration with St. Olav’s University Hospital in Trondheim. Although clinical research has high priority, the broad spectrum of systems for cancer studies provides translational research, covering ex vivo as well as in vivo MRI and MRS of cancer cells and laboratory animals. Bathen’s group also maintains several large biobanks of human tissue and biofluid samples.