In a recent study published in Nature Communications, researchers performed cellular, biochemical, and structural analyses to assess the multiple transferable resistance repressor (MtrR) binding and activation by male and female steroidal hormones, physiologically significant molecules interacting with gonococcal organisms during infection.
Neisseria gonorrhoeae is a gram-negative diplococcus that causes millions of diseases globally, including those transmitted sexually. There is no vaccination available, so reinfection is probable. Female patients may have pelvic inflammatory disease, ectopic pregnancy, infertility, or newborn blindness. The pathogen develops antibiotic resistance, and ceftriaxone is the only empirical therapy. However, ceftriaxone-resistant bacteria have been discovered in several countries, posing a substantial public health risk. The transcriptional regulator MtrR suppresses the mtrCDE operon, which colonizes the vaginal, rectal, and oral mucosa.
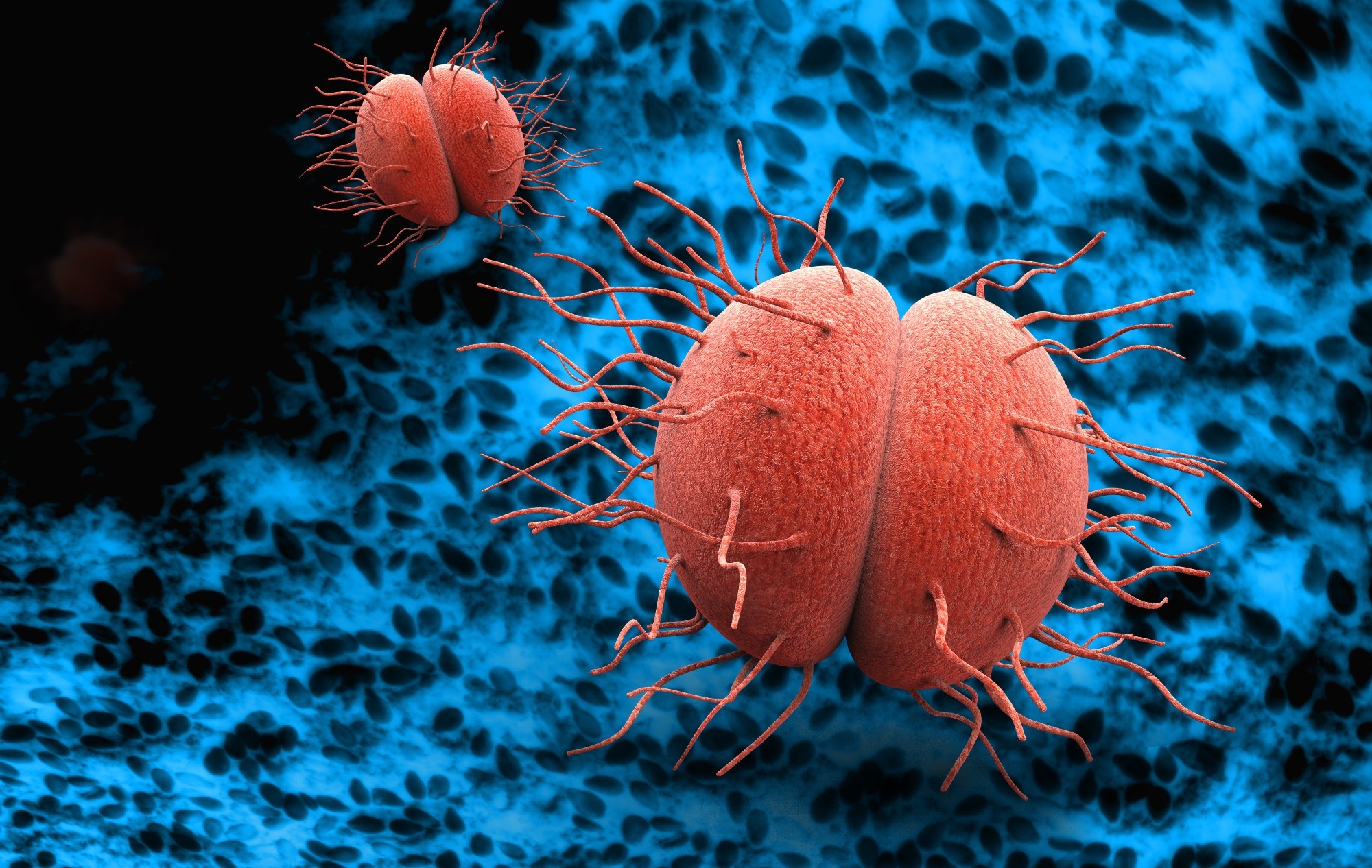 Study: Hormonal steroids induce multidrug resistance and stress response genes in Neisseria gonorrhoeae by binding to MtrR. Image Credit: Giovanni Cancemi / Shutterstock
Study: Hormonal steroids induce multidrug resistance and stress response genes in Neisseria gonorrhoeae by binding to MtrR. Image Credit: Giovanni Cancemi / Shutterstock
About the study
In the present study, researchers elucidated the binding and induction mechanisms of hormonal steroids by the MtrR transcriptional regulator that plays a crucial role in the multidrug resistance arsenal of Neisseria gonorrhoeae.
The researchers investigated the binding affinity of MtrR to specific ligands, hypothesizing that some MtrCDE ligands are inducers. They performed isothermal titration calorimetry (ITC) tests on β-estradiol (EST), progesterone (PTR), and testosterone (TES) to establish their affinity for MtrR. They also examined the binding of ethinyl estradiol (NDR), a synthetic estrogen used in hormonal contraception. To investigate whether host ligands cause biochemical induction of MtrR, they used a deoxyribonucleic acid (DNA) binding fluorescence polarization experiment to assess MtrR's binding affinity for rpoH and mtrCDE operators.
The team investigated the binding processes and structural foundation of MtrR concerning progesterone, β-estradiol, testosterone, and ethinyl estrogen. They established the structure of MtrR bound to EST at 2.4 Å resolution by de novo phasing and single-wavelength anomalous dispersion analysis. They also assessed the crystal structures of MtrR and steroids and the binding pocket of protomers unattached to the PTR. They introduced single-point mutations into the binding pocket of various residues to validate the attachment modalities.
The researchers investigated the binding characteristics of two mutants, W136A and R176E, MtrR W136L, and a Q133A substitution due to its side chain flexibility. They also investigated whether sublethal amounts of certain hormones may cause gonococcal resistance to antimicrobials in an MtrR-dependent manner. They found the minimum inhibitory concentration (MIC) values of steroidal hormones in the gonococcal strain FA19 and the range of hormone concentrations that do not impede gonococcal growth in liquid cultures. To test whether strain FA19's higher antimicrobial resistance (AMR) in the presence of sub-lethal doses of EST and PTR was due to increased expression of mtrCDE, they evaluated the in vivo expression of mtrC and an additional MtrR-repressed gene (rpoH).
Results
The study found that MtrR, a protein involved in cell metabolic control, binds to hormonal steroids such as progesterone, β-estradiol, and testosterone found in urogenital infection sites, and ethinyl estrogen, a component of various hormonal contraceptives. Steroid binding lowers MtrR affinity for cognate DNA, boosts mtrCDE expression, and improves antimicrobial resistance.
The crystal structures of MtrR coupled to these steroids show the binding processes and conformational changes that activate MtrR. Previous studies have demonstrated that mtrD gene mutations reduce the minimum inhibitory concentration of PTR in N. gonorrhoeae. Progesterone showed the highest efficacy in inhibiting gonococcal growth, making it a potent anti-gonococcal drug.
MtrR was bound to PTR, EST, and TES with dissociation constant (Kd) values of 2.8 µM, 1.7 µM, and 2.3 µM. Cholesterol, cortisol, and azithromycin exhibited no binding. The stoichiometry of TES and EST was one steroid for each monomer of MtrR and one PTR for each dimer of the multiple transferable resistance repressor.
NDR bound to the MtrR repressor with a dissociation constant of 0.9 µM. In FP tests, MtrR's binding affinity for mtrCDE operators and rpoH decreased by three-fold and 13-fold, respectively, compared to the affinity for binding in 1% MeOH presence alone. MtrR in higher concentrations attached non-specifically to DNA, which might explain the mtrCDE operator's smallfold increase in attachment over rpoH. The alignment of the MtrR-EST and MtrR-DNA structures showed three main motions that lead to protein induction.
The study findings showed that Neisseria gonorrhoeae, a multidrug-resistant bacteria, utilizes hormonal steroids such as β-estradiol, testosterone, ethinyl estrogen, and progesterone to colonize human organs. These hormones activate MtrCDE effluxes and RpoH stress responses via MtrR binding, allowing Neisseria gonorrhoeae to colonize human organs but not protect against gonococcal infection. The higher testosterone levels near infection sites show that these hormones might be harmful, helping bacteria to thrive by effluxing and activating genes involved in stress responses. Despite their efficacy in preventing unplanned pregnancies, these medications do not protect against gonococcal infections.
Journal reference:
- Hooks, G.M., Ayala, J.C., Holley, C.L., et al. Hormonal steroids induce multidrug resistance and stress response genes in Neisseria gonorrhoeae by binding to MtrR. Nat Commun 15, 1153 (2024), DOI: 10.1038/s41467-024-45195-1, https://www.nature.com/articles/s41467-024-45195-1