2. What should I know before I use Actrapid®, Protaphane® or Mixtard®?
Do not use if you have ever had an allergic reaction to insulin or any of the ingredients
listed at the end of the CMI.
Do not use if you are experiencing low blood sugar ("hypo") when your dose is due.
Talk to your doctor if you have any other medical conditions, take any other medicines,
or are pregnant or plan to become pregnant or are breastfeeding.
3. What if I am taking other medicines?
Some medicines may interfere with insulin and affect how it works.
4. How do I use Actrapid®, Protaphane® and Mixtard® Penfill®?
Carefully follow all instructions given to you by your doctor, nurse educator and
pharmacist regarding how to use your medicine, including preparing and injecting it.
5. What should I know while using Actrapid®, Protaphane® or Mixtard® Penfill®?
|
Things you should do
|
Remind any doctor, dentist or pharmacist you visit that you have diabetes and are
using insulin.
Monitor your blood sugar levels regularly
Carry some sugary food or fruit juice with you, in case you experience hypoglycaemia
("a hypo").
|
|
Things you should not do
|
Do not stop using this medicine unless directed by your doctor to.
Do not share your insulin or needles with anyone.
|
|
Driving or using machines
|
If your blood sugar is low or high, your concentration and ability to react might
be affected, and, therefore, also your ability to drive or operate machines.
|
|
Drinking alcohol
|
Alcohol may mask the symptoms of hypos. If you drink alcohol, your need for insulin
may change.
|
|
Looking after your medicine
|
Store Actrapid®, Mixtard® and Protaphane® Penfill® in the fridge between 2 and 8°C
Do not keep in a refrigerator, Penfill® that you are using, or that you are carrying
as a spare. You can use them up to 4 weeks after taking them out of the refrigerator.
Discard any unused insulin after 4 weeks.
|
6. Are there any side effects?
The most common side effect when using insulin is low blood sugar levels (a hypo).
Tell your relatives, friends, close workmates, teachers or carers that you have diabetes.
It is important that they can recognise the signs and symptoms of a hypo. For more
information, including what to do if you have any side effects, see Section
6. Are there any side effects? in the full CMI.
Active ingredients:
Insulin (rys)
Full Consumer Medicine Information (CMI)
This leaflet provides important information about using Actrapid® Penfill®, Protaphane®
Penfill® and/or Mixtard® 30/70 Penfill®. You should also speak to your doctor or pharmacist if you would like further information
or if you have any concerns or questions about using these medicines.
Where to find information in this leaflet:
1. Why am I using Actrapid®, Protaphane®, or Mixtard® Penfill®?
Actrapid® Penfill®; Protaphane® Penfill®; Mixtard® 30/70 Penfill® contain the active
ingredient insulin (rys).
Insulin (rys) is characterised by being identical to natural human insulin. The abbreviation
"rys" indicates the method of genetic engineering used to manufacture the insulin.
Actrapid®, Protaphane®, and Mixtard® Penfill® are used to treat diabetes mellitus.
Diabetes mellitus is a condition where your pancreas does not produce enough insulin
to control your blood sugar (glucose) level. Extra insulin is therefore needed.
There are two types of diabetes mellitus:
Type 1 diabetes
Type 2 diabetes
Patients with type 1 diabetes always require insulin to control their blood sugar
levels.
Some patients with type 2 diabetes may also require insulin after initial treatment
with diet, exercise and tablets is not enough.
Actrapid® is neutral insulin injection, a fast-acting insulin. This means that it
will start to lower your blood sugar level about half an hour after you inject it,
and the effect will last for approximately 8 hours.
Actrapid® Penfill ® can also used by doctors to treat some people with diabetes in
emergency situations. For emergency use, the insulin must first be withdrawn from
Penfill® into a syringe.
Actrapid® is often used in combination with longer-acting insulin products.
Protaphane® is isophane insulin injection, an intermediate-acting insulin. This means
that it will start to lower your blood sugar level about one and a half hours after
you inject it, and the effect will last for approximately 24 hours.
Protaphane® is often used in combination with fast- or rapid-acting insulin products.
Mixtard® 30/70 is two-phase isophane insulin injection, and is a mixture of fast-
and longer-acting insulins. Mixtard® 30/70 will start to lower your blood sugar level
about half an hour after you inject, and the effect will last for approximately 24
hours.
As with all insulins, the duration of action will vary according to the type of insulin,
the dose, injection site, blood flow, temperature and level of physical activity.
Insulin is not addictive. Insulin is available only with a doctor’s prescription.
2. What should I know before I use Actrapid®, Protaphane® or Mixtard®?
Warnings
Do not use Actrapid®, Protaphane® or Mixtard® Penfill®:
if you are allergic to insulin, or any product containing insulin, or any of the ingredients
listed at the end of this leaflet.
if you are experiencing low blood sugar level (a "hypo") when your dose is due.
if the expiry date printed on the pack has passed, or if the packaging is torn or
shows signs of tampering.
in insulin infusion pumps.
Do not inject Protaphane® or Mixtard® 30/70 into a vein.
Check with your doctor if you:
are experiencing a lot of hypos, and follow their advice
have any other medical conditions, such as: kidney liver, adrenal gland, pituitary
gland or thyroid gland problems
take any medicines for any other condition
have an infection or fever
are planning to travel.
During treatment, you may be at risk of developing certain side effects. It is important
you understand these risks and how to monitor for them. See additional information
under Section
6. Are there any side effects?
Pregnancy and breastfeeding
Check with your doctor if you are pregnant or intend to become pregnant. Pregnancy
can make managing your diabetes more difficult, and may require adjustment of how
much insulin you need.
Talk to your doctor if you are breastfeeding or intend to breastfeed.
Heart disease or a history of stroke
Tell your doctor as soon as possible if you experience signs of heart failure such
as unusual shortness of breath or rapid increase in weight or localised swelling (oedema).
Some patients with long-standing type 2 diabetes mellitus and heart disease or previous
stroke, and who are treated with a class of medicines known as thiazolidinediones
in combination with insulin can develop heart failure.
3. What if I am taking other medicines?
Tell your doctor or pharmacist if you are taking any other medicines, including any
medicines, vitamins or supplements that you buy without a prescription from your pharmacy,
supermarket or health food shop.
Some medicines may interfere with insulin and affect how it works.
Medicines that may
increase
the effect of insulin, and therefore reduce insulin requirements include:
other medicines used to treat type 2 diabetes
octreotide - used to treat gastrointestinal endocrine tumours and enlargement of parts
of the body (e.g. hands, feet, head) caused by abnormal growth hormone levels
lanreotide - used to treat enlargement of parts of the body (e.g. hands, feet, head)
caused by abnormal hormone levels
monoamine oxidase inhibitors (MAOIs) - used to treat depression
non-selective beta-blockers - used to treat certain heart conditions and high blood
pressure
alpha-blockers - used to treat high blood pressure and to relieve difficulty in passing
urine caused by an enlarged prostate
angiotensin converting enzyme (ACE) inhibitors - used to treat certain heart conditions,
high blood pressure and elevated protein/albumin in the urine
salicylates, e.g. aspirin - used to relieve pain and lower fever
anabolic steroids - used to promote growth
quinine - used to treat malaria and relieve muscle cramps
quinidine - used to treat heart problems
sulphonamides - a type of antibiotic used to treat bacterial infections.
Medicines that may
reduce
the effect of insulin, and increase the insulin requirements include:
oral contraceptives ("the pill") - used for birth control
thiazides, frusemide or ethacrynic acid - used to treat high blood pressure or fluid
retention (oedema)
glucocorticoids (except when applied locally) - used to treat inflammatory conditions
thyroid hormones - used to treat malfunction of the thyroid gland
sympathomimetics - used to treat asthma
octreotide - used to treat gastrointestinal endocrine tumours and enlargement of parts
of the body (e.g. hands, feet, head) caused by abnormal growth hormone levels
lanreotide - used to treat enlargement of parts of the body (e.g. hands, feet, head)
caused by abnormal hormone levels
growth hormone - used to treat growth disorders
diazoxide - used to treat high blood pressure
asparaginase - used to treat leukaemia and lymph gland tumours
nicotinic acid - used to treat high cholesterol levels in the blood
oxymetholone - used to treat certain blood disorders
danazol - used to treat endometriosis, menorrhagia, fibrocystic breast disease and
hereditary angioedema.
Check with your doctor or pharmacist if you are not sure about what medicines, vitamins
or supplements you are taking and if these affect
Actrapid®, Protaphane® or Mixtard®
4. How do I use Actrapid®, Protaphane® and Mixtard Penfill®?
How much to use
Carefully follow all instructions given to you by your doctor, nurse educator and
pharmacist regarding how to use your medicine.
Your doctor or diabetes education nurse will tell you how much of this medicine you
need to use each day.
It is very important that you manage your diabetes carefully. Too much or too little
insulin can cause serious effects.
When to use Actrapid®, Protaphane®, Mixtard® Penfill®?
Your doctor or diabetes education nurse will tell you when and how often to inject
your insulin.
How to inject Actrapid®, Protaphane®, Mixtard® Penfill®?
Penfill® cartridges are designed to be used with Novo Nordisk insulin delivery devices
(such as NovoPen®), and NovoFine® needles.
Make sure you are using the correct type and strength of insulin.
Carefully follow the instructions on how to use your Penfill® in the Novo Nordisk
insulin delivery device.
If you use more than one type of insulin in a Penfill®, you must use a separate insulin
delivery device for each type.
Do not use the insulin level indicator on the device to measure your dose of insulin.
Inject insulin under the skin (subcutaneous injection) as shown to you by your doctor
or diabetes education nurse.
Take care not to drop or knock the device that contains Penfill®.
Checking your Penfill® before injection
Check your Penfill® every time you are preparing your injection to make sure you are
using the correct type and strength of insulin.
Disinfect the rubber membrane with a medicinal swab.
Do not use your Actrapid® Penfill® unless the insulin appears clear and colourless.
Do not use it if the insulin appears thickened or has bits in it.
Do not use your Protaphane® or Mixtard® 30/70 Penfill® if the insulin is no longer
a cloudy, white suspension after mixing, or if it has bits in it.
Do not use your Penfill® if you notice any damage, including any damage to the rubber
plunger (stopper) or if there is a gap between the plunger and the white label band.
Preparing your Penfill® for injection
On the Penfill® cartridge is a coloured band. Do not start an injection with a Penfill®
cartridge if you have emptied beyond the coloured band.
The glass ball must have adequate space to resuspend the insulin. Resuspending is
easier when the insulin has reached room temperature.
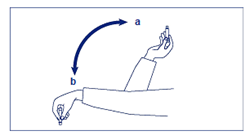
Before you put Penfill® into the Novo Nordisk insulin delivery device, move it up
and down between positions a and b - see picture below - so that the glass ball in
the cartridge moves from one end to the other at least 20 times. The movement must
always be repeated until the liquid appears uniformly white and cloudy.
If Penfill® is already inside the Novo Nordisk insulin delivery device, turn the delivery
device upside-down at least 10 times with the cartridge inside it. Do this again before
every injection.
Complete the remaining stages of injection without delay.
Checking for insulin flow (priming):
Always check your Novo Nordisk insulin delivery device for insulin flow (priming)
before each injection, as described in the device user manual.
The priming procedure may highlight a malfunction with your insulin delivery device.
Priming also removes any air bubbles and helps indicate whether or not a needle is
broken.
Only dial up your required dose after you see a drop of insulin at the needle tip.
After priming, if you need to put the insulin delivery device down, make sure the
needle does not touch anything.
Choose a site for injection
Inject the medicine into the abdomen, thighs, upper arms or buttocks. Note that your insulin will work more quickly if you inject into the abdomen.
Change the injection site so that the same position is not used more often than once
a month. This reduces the risk of developing lumps or skin pitting.
Pinch the skin between two fingers, push the needle into the raised skin, and inject
the full dose of insulin under the skin.
Slowly count to 6 before pulling the needle out.
Keep the push button fully depressed until the needle has been withdrawn.
Apply gentle pressure over the injection site for several seconds
Do not rub the area
After injecting:
Dispose of your used needle safely into a yellow plastic sharps container after each
injection.
If you are using Actrapid® or Mixtard®, it is recommended that you eat a meal or a
snack containing carbohydrate within 30 minutes of the injection.
Do not share needles, insulin cartridges or insulin delivery devices.
If you forget to inject your insulin - hyperglycaemia
Actrapid®, Protaphane® and Mixtard Penfill® must be used strictly as advised by your
doctor or nurse educator.
If you forget your insulin dose, test your blood sugar level as soon as possible.
If you are not sure what to do, talk to your doctor, diabetes education nurse or pharmacist.
Do not use a double dose of your insulin.
If it is almost time for your next dose, skip the dose you missed and inject your
next dose when you are meant to.
Otherwise, use it as soon as you remember and then go back to using it as you would
normally.
If you are using Actrapid® or Mixtard®, make sure you eat some carbohydrate within
30 minutes of the injection.
If you use too much insulin - hypoglycaemia
If you think that you have used too much insulin, you may need urgent medical attention.
You should immediately:
phone the Poisons Information Centre
(by calling
13 11 26), or
contact your doctor, or
go to the Emergency Department at your nearest hospital.
You should do this even if there are no signs of discomfort or poisoning.
5. What should I know while using Actrapid®, Protaphane® or Mixtard® Penfill®?
Hypoglycaemia
Your blood sugar level may become too low (you may experience hypoglycaemia (a hypo)
if you:
accidentally use too much of this medicine
have too much or unexpected exercise
delay eating meals or snacks
eat too little food
are ill.
The first symptoms of mild to moderate hypos can come on suddenly. They may include:
cold sweat, cool pale skin
fatigue, drowsiness, unusual tiredness and weakness
nervousness, feeling anxious, tremor, rapid heart beat
confusion, difficulty concentrating
excessive hunger
vision changes
headache, nausea.
Always carry some sugary food or fruit juice with you.
Do not inject any insulin if you feel a hypo coming on.
Tell your relatives, friends, close workmates or carers that you have diabetes. It
is important that they recognise the signs and symptoms of a hypo.
Make sure they know to give you some sugary food or fruit juice for mild to moderate
symptoms of a hypo.
If you lose consciousness, make sure they know:
to turn you on your side and get medical help immediately
not to give you anything to eat or drink as you may choke.
An injection of the hormone glucagon may speed up recovery from unconsciousness. This
can be given by a relative, friend, workmate or carer who knows how to give it.
If glucagon is used, eat some sugary food or have a sugary
drink as soon as you are conscious again.
If you do not feel better after this, contact your doctor, diabetes education nurse,
or the closest hospital.
See your doctor if you keep having hypo reactions, or if you have ever become unconscious
after using insulin.
Your insulin dose may need to be changed.
If a severe hypo is not treated, it can cause convulsions, brain damage and even death.
Hyperglycaemia
Your blood sugar levels may become high (hyperglycaemia) if you:
miss doses of insulin or use less insulin than you need
have uncontrolled diabetes
exercise less than usual
eat more carbohydrates than usual
are ill or stressed.
High blood sugar levels over a long period of time can lead to too much acid in the
blood (diabetic ketoacidosis).
Contact your doctor immediately if your blood sugar level is high or you recognise
any of the following symptoms.
Symptoms of mild to moderate hyperglycaemia include:
drowsy feeling
flushed face
thirst, loss of appetite
fruity odour on the breath
blurred vision
passing larger amounts of urine than usual
getting up at night more often than usual to pass urine
high levels of glucose and acetone in the urine.
Symptoms of severe hyperglycaemia include:
heavy breathing
fast pulse
nausea, vomiting
dehydration
loss of consciousness.
Severe hyperglycaemia can lead to unconsciousness and in extreme cases death if untreated.
Things you should do
Measure your blood sugar levels regularly.
Make sure all friends, relatives, workmates or carers know that you have diabetes.
If your child has diabetes, it is important to tell their teachers and carers.
Keep using your insulin even if you feel well. It helps to control your diabetes, but does not cure it.
Always carry some sugary food or fruit juice with you.
Tell your doctor if you are feeling sick, especially if you are experiencing nausea
or vomiting.
Tell your doctor if you have trouble recognising the symptoms of hypos.
Remind any doctor, dentist or pharmacist you visit that you have diabetes and are
using insulin.
Tell your doctor if your diet changes or you are exercising more.
Tell your doctor if you notice any skin changes at the injection site.
The injection site should be rotated to help prevent changes to the fatty tissue under
the skin, such as skin thickening, skin shrinking or lumps under the skin. The insulin
may not work very well if you inject into a lumpy, shrunken or thickened area. Change
the injection site with each injection to help prevent these skin changes.
Things you should not do
Do not stop using your insulin unless your doctor tells you to.
Do not give your insulin to anyone else, even if they have diabetes.
Do not share needles.
Driving or using machines
Be careful before you drive or use any machines or tools until you know how the insulin
affects you.
If your blood sugar is low or high your concentration and ability to react might be
affected, and therefore also your ability to drive or operate a machine.
Bear in mind that you could endanger yourself or others. Please ask your doctor whether
you can drive a car, especially if:
• you have frequent hypos
• you find it hard to recognise hypos.
Drinking alcohol
Tell your doctor if you drink alcohol.
Alcohol may mask the signs of a hypo. Carefully monitor your blood sugar levels when
drinking.
Looking after your medicine
Penfill® cartridges that are not being used should be stored between 2°C and 8°C in
the refrigerator (away from the cooling element).
Penfill® cartridges that you are using, or that you are carrying as a spare, should
not be kept in a refrigerator.
Protect the insulin in Penfill® from light by keeping the cartridges in the carton
when not in use.
Do not allow cartridges to be frozen, or exposed to excessive heat and light.
Never use Actrapid® Penfill® if the solution is not clear and colourless.
Never use Protaphane® or Mixtard® Penfill® if the suspension does not become white
and uniformly cloudy after resuspending.
Keep it where young children cannot reach it.
In an emergency Actrapid® is suitable for injection into a muscle (intramuscular administration)
or into a vein (intravenous administration) but only by a doctor. It must be withdrawn
from the cartridge and given by a needle and syringe.
Discard any insulin left after emergency use.
When to discard your medicine
You can use Actrapid®, Mixtard® and Protaphane® Penfill® for up to 4 weeks after taking
it out of the refrigerator if kept below 25°C.
Discard Penfill® cartridges after 4 weeks even if there is still some insulin left
in them.
Getting rid of unwanted medicine
If you no longer need to use this medicine or it is out of date, take it to any pharmacy
for safe disposal.
Never use insulin after the expiry date printed on the Penfill® label and carton after
'Expiry'. The expiry date refers to the last day of that month.
6. Are there any side effects?
All medicines can have side effects. If you do experience any side effects, most of
them are minor and temporary. However, some side effects may need medical attention.
See the information below and, if you need to, ask your doctor or pharmacist if you
have any further questions about side effects.
Less serious side effects
Serious side effects
Tell your doctor or pharmacist if you notice anything else that may be making you
feel unwell.
Other side effects not listed here may occur in some people.
Reporting side effects
After you have received medical advice for any side effects you experience, you can
report side effects to the Therapeutic Goods Administration online at
www.tga.gov.au/reporting-problems . By reporting side effects, you can help provide more information on the safety of
this medicine.
Always make sure you speak to your doctor or pharmacist before you decide to stop
taking any of your medicines.
7. Product details
This medicine is only available with a doctor's prescription.
What Actrapid® Penfill® contains
|
Active ingredient
(main ingredient)
|
Insulin (rys) 100 IU/mL
|
|
Other ingredients
(inactive ingredients)
|
glycerol
metacresol
zinc chloride
Water for Injection.
hydrochloric acid and sodium hydroxide to adjust the pH.
|
Do not take this medicine if you are allergic to any of these ingredients.
What Protaphane® Penfill® contains
|
Active ingredient
(main ingredient)
|
Isophane insulin (rys) 100 IU/mL
|
|
Other ingredients
(inactive ingredients)
|
glycerol
metacresol
phenol
dibasic sodium phosphate dihydrate
zinc chloride
protamine sulfate
Water for Injection.
hydrochloric acid and sodium hydroxide to adjust the pH.
|
|
Potential allergens
|
protamine sulfate is derived from fish
|
Do not take this medicine if you are allergic to any of these ingredients.
What Mixtard® 30/70 Penfill contains
|
Active ingredient
(main ingredient)
|
a pre-mixed neutral suspension of insulin (rys) 100 IU/mL, consisting of neutral insulin injection (30%) and isophane insulin injection
(70%)
|
|
Other ingredients
(inactive ingredients)
|
glycerol
metacresol
phenol
dibasic sodium phosphate dihydrate
zinc chloride
protamine sulfate
Water for Injection.
hydrochloric acid and sodium hydroxide to adjust the pH.
|
|
Potential allergens
|
protamine sulfate is derived from fish
|
Do not take this medicine if you are allergic to any of these ingredients.
What Actrapid®, Protaphane® and Mixtard® Penfill® look like
A coloured band is located on the Penfill® cartridge. The colour of the band is specific
for the insulin preparation.
Actrapid® is a clear, colourless solution for subcutaneous injection. Actrapid® Penfill®
3 mL is a glass cartridge (AUST R 169623)
Protaphane® Penfill® is a white, cloudy suspension for subcutaneous injection. Protaphane®
Penfill® 3 mL is a class cartridge (AUST R 169635)
Mixtard® 30/70 is a white, cloudy suspensions for subcutaneous injection. Penfill®
3mL is a glass cartridge (AUST R 169629)
Who distributes these medicines?
Actrapid® Penfill®, Protaphane® Penfill® and Mixtard® 30/70 Penfill® are supplied
in Australia by:
Novo Nordisk Pharmaceuticals Pty Ltd
Level 10
118 Mount Street
North Sydney NSW 2060
Australia
Further information
For further information call Novo Nordisk Medical Information on 1800 668 626.
You can also get more information about diabetes from
Diabetes Australia:
freecall helpline 1300 136 588
Actrapid®, Protaphane®, Mixtard®, NovoPen®, NovoFine® and Penfill® are registered
trademarks of Novo Nordisk A/S.
© 2025
Novo Nordisk A/S
This leaflet was prepared in October 2025