2. What should I know before I use COPAXONE PEN?
Do not use if you have ever had an allergic reaction to glatiramer acetate or any
of the ingredients listed at the end of the CMI.
Talk to your doctor if you have any other medical conditions, take any other medicines,
or are pregnant or plan to become pregnant or are breastfeeding.
3. What if I am taking other medicines?
Some medicines may interfere with COPAXONE PEN and affect how it works.
4. How do I use COPAXONE PEN?
The recommended dose of COPAXONE PEN is one 40 mg/mL pre-filled pen (1mL) injected
three times a week and at least 48 hours apart.
COPAXONE PEN 40 mg/mL is given by an injection into the fatty layer under the skin
(subcutaneous injection).
5. What should I know while using COPAXONE PEN?
|
Things you should do
|
Remind any doctor, dentist or pharmacist you visit that you are using COPAXONE PEN.
|
|
Things you should not do
|
Do not use more than the recommended dose unless your doctor tells you to.
|
|
Looking after your medicine
|
Keep COPAXONE PEN 40 mg/mL in the refrigerator at 2°C to 8°C.
Keep COPAXONE PEN 40 mg/mL in the pack until it is time to use it. Protect from direct
light.
|
6. Are there any side effects?
Common side effects: Immediate Post Injection Reaction which includes the following
symptoms - reddening of the face and/or neck, chest pain or tightness, feeling your
heart beat quickly (heart palpitations), anxiety and difficulty in breathing.
Serious side effects: Symptoms of an allergic reaction that include - swelling of
the face, lips, mouth or throat, which may cause difficultly in swallowing or breathing,
hives, chest pain, trouble breathing and severe pain, redness or swelling at the injection
site that does not go away.
Solution for Injection
Active ingredient(s):
glatiramer acetate
Full Consumer Medicine Information (CMI)
This leaflet provides important information about using COPAXONE PEN 40 mg/mL. You should also speak to your doctor or pharmacist if you would like further information
or if you have any concerns or questions about using COPAXONE PEN.
Where to find information in this leaflet:
1. Why am I using COPAXONE PEN?
COPAXONE PEN contains the active ingredient glatiramer acetate. The exact mechanism of how Copaxone works is unknown, it is thought that Copaxone
works by changing the immune processes that are believed to be responsible for the
disease.
COPAXONE PEN 40 mg/mL is used for the management of relapsing forms of Multiple Sclerosis
(MS).
COPAXONE PEN may also be used in patients who, for the first time, have experienced
symptoms and have MRI changes that indicate a high risk for development of MS. Your
doctor will rule out any other reasons which could explain these symptoms before you
are treated.
The cause of MS is not yet known. MS affects the brain and spinal cord. In MS, the
body’s immune system reacts against its own myelin (the ‘insulation’ surrounding nerve
fibres). In relapsing forms of MS, people can have ‘exacerbations’ from time to time
(e.g. blurred vision, weakness in the legs or arms, or loss of control of bowel or
bladder function). These are followed by periods of recovery.
Copaxone has been shown to be effective in reducing the number of relapses in patients
with relapsing remitting MS. Although it is not a cure, patients treated with COPAXONE
PEN 40mg/mL generally find that they will experience fewer relapses.
2. What should I know before I use COPAXONE PEN?
Warnings
Copaxone can cause severe allergic reactions, some of which may be life-threatening.
These reactions may occur shortly after administration, even months or years after
starting treatment and even if previous administrations were without allergic reactions.
The signs and symptoms of allergic reactions may overlap with post-injection reactions.
Do not use COPAXONE PEN if:
you are allergic to glatiramer acetate, or any of the ingredients listed at the end
of this leaflet.
Always check the ingredients to make sure you can use this medicine.
Check with your doctor if you:
have any other medical conditions including asthma and liver disease
take any medicines for any other condition
have ever had asthma
have a history of severe allergic reactions
have ever had a liver injury
plan to have surgery
During treatment, you may be at risk of developing certain side effects. It is important
you understand these risks and how to monitor for them. See additional information
under Section
6. Are there any side effects?
Pregnancy and breastfeeding
Check with your doctor if you are pregnant or intend to become pregnant.
Limited data in humans showed no negative effects of glatiramer acetate on breastfed
infants.
Talk to your doctor if you are breastfeeding or intend to breastfeed.
Children
Do not give Copaxone to children. There is no experience with its use in children
under 12 years of age.
3. What if I am taking other medicines?
Tell your doctor or pharmacist if you are taking any other medicines, including any
medicines, vitamins or supplements that you buy without a prescription from your pharmacy,
supermarket or health food shop.
Some medicines may interfere with Copaxone and affect how it works.
Some medicines may interfere with the absorption of Copaxone.
Check with your doctor or pharmacist if you are not sure about what medicines, vitamins
or supplements you are taking and if these affect COPAXONE PEN.
4. How do I use COPAXONE PEN?
How much to use
The recommended dose of COPAXONE PEN is one 40 mg/mL pre-filled pen (1mL) injected
three times a week and at least 48 hours apart.
Follow the instructions provided and use COPAXONE PEN until your doctor tells you
to stop.
When to use COPAXONE PEN
COPAXONE PEN 40 mg/mL should be used, if possible, at the same time and on the same
three days each week (for example, Monday, Wednesday and Friday) at least 48 hours
apart.
Do not change the dose or dosing schedule or stop using COPAXONE PEN without talking
to your doctor.
How to use COPAXONE PEN
COPAXONE PEN 40 mg/mL is given by an injection into the fatty layer under the skin
(subcutaneous injection).
Many people with MS learn to give themselves the injection or have it given by a carer.
Self-injection needs to be taught and practiced. It is important that a qualified
healthcare professional supervises your first injection.
Your doctor may teach you to self-inject or arrange for an MS education nurse to do
so.
You may have a friend attend the injection training session as your assistant. Especially
when you first start giving yourself injections, your assistant should be with you.
Talk to your doctor or your nurse or telephone 1800 288 382 in Australia
or 0800 800 097 in New Zealand for more information
.
After being taught to self-inject, you can refer to this leaflet for step-by-step
instructions about how to prepare and inject COPAXONE PEN 40 mg/mL.
The following instructions explain how to inject COPAXONE PEN 40 mg/mL yourself.
Do not attempt self-injection until you are confident that you understand how to inject
yourself.
Please read these instructions carefully.
Before you inject
COPAXONE PEN 40 mg/mL pre-filled pen is pre-mixed and ready for you to use.
Make sure that the pen is taken out of the refrigerator for 20 minutes before you
use it.
It is important that the solution is at room temperature when you inject it. If you
need to delay your injection, return the pen to its original carton in the refrigerator.
Do not attempt to remove the syringe from the Pen device.
Always inspect
COPAXONE PEN solution in the pre-filled pen before you use it. Do not inject the solution
if it is cloudy or has particles in it.
Do not use if the cap has been removed or damaged.
Gathering the Materials
Gather the following items on a towel that is laid on a flat surface in a clean, well-lit
area:
One COPAXONE PEN 40 mg/mL (at room temperature - as described above)
A dry cotton ball
An alcohol swab
Disposal unit for used pens (such as a sharps container)
Wash and dry your hands. Do not touch your hair or skin afterwards. This will help
prevent infection.
Deciding where to Inject
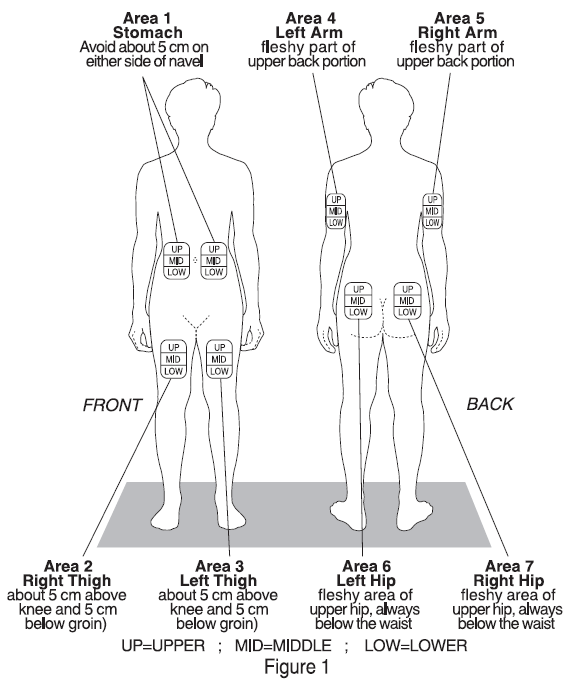
There are seven injection areas on your body; arms, thighs, back of the hips and stomach
(belly). Within each injection area there are multiple injection sites (Figure 1).
Rotate the injection sites within an area.
You should not use any site more than once a week. Choose a different site for each
injection. This will reduce the likelihood of irritation, pain or loss of fatty tissue
(lipoatrophy) at the site of injection.
Marking a calendar will help you keep track of the sites you have used each week.
Do not inject in an area of skin that is bruised, inflamed or damaged.
Giving yourself the injection
Do not administer COPAXONE PEN 40 mg/mL by any other method or route other than subcutaneous
injection using the technique as demonstrated by your doctor in accordance with this
leaflet or the separate "Instructions for use” guide.
Speak to your doctor if you are unsure.
Do not reuse the pen. Each pen should be used only for one injection.
Refer to the "Instructions for Use" leaflet with this medicine for helpful hints on
where you should inject if you are unsure.
If you forget to use COPAXONE PEN
COPAXONE PEN should be used regularly at the same time and on the same three days
each week. If you miss your dose at the usual time, you should take your next dose
as soon as you remember or are able to take it, then skip the following day. If possible,
you should return to your regular administration schedule the following week.
Do not take a double dose to make up for the dose you missed.
If you use too much COPAXONE PEN
If you think that you have used too much COPAXONE PEN, you may need urgent medical
attention.
You should immediately:
phone the Poisons Information Centre
(by calling 13 11 26 in Australia or 0800 764 766 in New Zealand), or
contact your doctor, or
go to the Emergency Department at your nearest hospital.
You should do this even if there are no signs of discomfort or poisoning.
5. What should I know while using COPAXONE PEN?
Things you should do
If you are about to be started on any new medicine, tell your doctor and pharmacist
that you are using COPAXONE PEN 40 mg/mL.
If you plan to have surgery that needs a general anaesthetic, tell your doctor or
dentist that you are using this medicine.
If you become pregnant while you are using this medicine, talk to your doctor to discuss
whether ongoing COPAXONE PEN treatment is appropriate for you.
Remind any doctor, dentist or pharmacist you visit that you are using COPAXONE PEN.
Things you should not do
Do not use more than the recommended dose unless your doctor tells you to.
Do not give this medicine to anyone else, even if they have the same condition as
you.
Looking after your medicine
Keep COPAXONE PEN 40 mg/mL in the refrigerator at 2°C to 8°C.
Keep COPAXONE PEN 40 mg/mL in the pack until it is time to use it. Protect from direct
light.
In the event of refrigeration being unavailable, COPAXONE PEN 40 mg/mL may be stored
between 15°C - 25°C on one occasion for up to one month.
COPAXONE PEN 40 mg/mL must not be frozen. Do not place in the freezer or freezing
compartment of a refrigerator.
Follow the instructions in the carton on how to take care of your medicine properly.
Store it in a cool dry place away from moisture, heat or sunlight; for example, do
not store it:
in the bathroom or near a sink, or
in the car or on window sills.
Keep it where young children cannot reach it.
When to discard your medicine
Ask your doctor or nurse about obtaining a “sharps container”.
After use, place all used pens in a hard-walled plastic container, such as a liquid
laundry detergent container or sharps container.
It is very important that you keep the cover of the container tightly shut and that
you store it out of the reach of children. When the container is full, check with
your doctor or nurse about proper disposal.
Getting rid of any unwanted medicine
If you no longer need to use this medicine or it is out of date, take it to any pharmacy
for safe disposal.
Do not use this medicine after the expiry date.
6. Are there any side effects?
All medicines can have side effects. If you do experience any side effects, most of
them are minor and temporary. However, some side effects may need medical attention.
See the information below and, if you need to, ask your doctor or pharmacist if you
have any further questions about side effects.
Less serious side effects
|
Less serious side effects
|
What to do
|
|
Skin related:
pain, redness, itching, hardening of the skin or an infection at the site where you
have injected yourself
Immediate Post Injection Reaction which includes the following symptoms:
reddening of the face and/or neck,
chest pain or tightness,
feeling your heart beat quickly (heart palpitations),
anxiety and difficulty in breathing
allergic reaction (anaphylactic).
Gut related:
nausea (feeling sick)
constipation
Symptoms related to liver injury:
yellowing of the skin or eyes
dark urine
abdominal pain
vomiting
loss of appetite
weight loss
unusual tiredness
Other:
pain in the joints
sore muscles
feeling of weakness
dizziness
|
Speak to your doctor if you have any of these less serious side effects and they worry
you.
|
Serious side effects
Tell your doctor or pharmacist if you notice anything else that may be making you
feel unwell.
Other side effects not listed here may occur in some people.
Reporting side effects
After you have received medical advice for any side effects you experience, you can
report side effects to the Therapeutic Goods Administration at
www.tga.gov.au/reporting-problems . By reporting side effects, you can help provide more information on the safety of
this medicine.
Always make sure you speak to your doctor or pharmacist before you decide to stop
taking any of your medicines.
7. Product details
This medicine is only available with a doctor's prescription.
What COPAXONE PEN contains
|
Active ingredient
(main ingredient)
|
Glatiramer acetate 40 mg/mL
|
|
Other ingredients
(inactive ingredients)
|
Mannitol
Water for Injections
|
Do not take this medicine if you are allergic to any of these ingredients.
What COPAXONE PEN looks like
COPAXONE PEN 40 mg/ml consists of a single use, disposable, spring-powered pen injector
with needle safety shield integrating a 1 ml glass single use pre-filled syringe with
a staked ½ inch needle. The pre-filled syringe contains glatiramer acetate which is
a clear colourless solution (Aust R 316728).
COPAXONE PEN 40 mg/mL are supplied in packs containing 3, 12 or 36 pre-filled pens.
Not all pack sizes may be marketed.
Who distributes COPAXONE PEN
COPAXONE PEN 40 mg/mL is distributed in Australia by:
Teva Pharma Australia Pty Ltd
Level 1, 37 Epping Road
Macquarie Park NSW 2113
COPAXONE PEN 40 mg/mL is distributed in New Zealand by:
Teva Pharma (New Zealand) Limited
PO Box 128 244
Remuera
Auckland 1541
This leaflet was prepared in December 2024.
® Copaxone Pen is a registered trademark of Teva Pharmaceuticals Industries Ltd.