2. What should I know before I use Trisequens®?
Do not use if you have ever had an allergic reaction to Trisequens® or any of the
ingredients listed at the end of the CMI.
Talk to your doctor about your medical history and your family’s medical history,
and if you take any other medicines, before starting Trisequens®. Do not use if pregnant
or plan to become pregnant or are breastfeeding.
3. What if I am taking other medicines?
Some medicines may interfere with Triseqens® and affect how it works.
4. How do I use Trisequens®?
Trisequens® must be taken once a day, at about the same time each day.
It is supplied in a 28-day calendar dial pack.
5. What should I know while using Trisequens®?
|
Things you should do
|
Remind any doctor, dentist or pharmacist you visit that you are using Trisequens®.
Keep all of your doctor's appointments so that you can be carefully monitored.
|
|
Things you should not do
|
Do not stop using this medicine suddenly.
Do not change the way you take Trisequens®.
|
|
Driving or using machines
|
There is no specific information on driving or using machines while you are taking
Trisequens®.
|
|
Drinking alcohol
|
There is no specific information on the effect of drinking alcohol while you are taking
Trisequens®
|
|
Looking after your medicine
|
Keep Trisequens® in a cool, dark place where the temperature stays below 25°C.
|
6. Are there any side effects?
Serious side effects may include the potential for blood clots (in veins, lungs or
brain), severe allergic reaction (anaphylaxis), sudden onset headache or migraine,
changes to breasts suggestive of breast cancer, unexpected vaginal bleeding.
|
WARNING:
Estrogens and progestogens should not be used for the prevention of heart attacks,
stroke or dementia.
A large study called the Women’s Health Initiative reported that women who took these
hormones in combination or alone after menopause, compared to a placebo (a medicine
with no active ingredient), had an increased risk of heart attacks and strokes, breast
cancer, blood clots in the lungs or legs, and a higher risk of developing dementia
(memory loss) in older women.
Any estrogen with or without progestogen should be prescribed at the lowest effective
dose and for the shortest duration determined by considering the risk and benefits
for you as an individual. Speak to your doctor if you have any questions.
|
Active ingredients:
estradiol hemihydrate and norethisterone acetate
Full Consumer Medicine Information (CMI)
This leaflet provides important information about using Trisequens®. You should also speak to your doctor or pharmacist if you would like further information
or if you have any concerns or questions about using Trisequens®
Where to find information in this leaflet:
1. Why am I using Trisequens®?
Trisequens® contains the active ingredient estradiol hemihydrate (an estrogen) and
norethisterone acetate (a progestogen).
Trisequens® is a hormone replacement therapy (HRT). It is used for short-term relief
of some of the symptoms of menopause.
2. What should I know before I use Trisequens®?
Medical history and regular check-ups
The use of HRT carries risks which need to be considered when deciding whether to
start taking it, or whether to carry on taking it.
Before you start (or restart) HRT, your doctor must ask about your own and your family´s
medical history. Your doctor may decide to perform a physical examination. This may
include an examination of your breasts and/or an internal examination, if necessary.
Note: Trisequens® is not a contraceptive. If it is less than 12 months since your
last menstrual period or you are under 50 years' old, you may still need to use additional
contraception to prevent pregnancy.
Speak to your doctor before starting Trisequens® if you have any questions or concerns.
Warnings
Do not use Trisequens® if:
you have, have had or suspect having breast cancer
you have, have had or suspect having cancer of the uterus lining (endometrial cancer),
or any other estrogen dependent cancer
you have any unexplained vaginal bleeding
you have excessive thickening of the uterus lining (endometrial hyperplasia) that
is not being treated
you have or have ever had a blood clot in a vein (venous thromboembolism), such as
in the legs (e.g. deep vein thrombosis), or the lungs (pulmonary embolism)
you have a blood clotting disorder (such as protein C, protein S or antithrombin deficiency)
you have or previously have had a disease caused by blood clots in the arteries, such
as a heart attack, stroke or angina
you have or have ever had a liver disease, and your blood test results have not returned
to normal
you have a rare blood problem called 'porphyria' which is passed down in families
(inherited)
you are pregnant or suspect you may be pregnant, or you are breastfeeding
you are allergic to estradiol or norethisterone, or any of the ingredients listed
at the end of this leaflet. Always check the ingredients to make sure you can use
this medicine.
Check with your doctor if you:
have premature menopause
have fibroids or a growth of the uterus lining outside your uterus (endometriosis)
have a history of excessive growth of the uterus lining (endometrial hyperplasia)
have an increased risk of developing blood clots (see Blood clots in a vein (venous thromboembolism)
are to be hospitalised or undergoing surgery, particularly where you are or will be
off your feet for a long time. You may need to stop taking Trisequens® for several
weeks before your operation, to reduce the risk of a blood clot
have an increased risk of getting an estrogen-sensitive cancer (such as having a mother,
sister or grandmother who has had breast cancer)
have high blood pressure
have a liver disorder, such as a benign liver tumour
have diabetes
have or have had gallstones
have migraines or severe headaches
have systemic lupus erythematosus (SLE)
have epilepsy
have asthma
have otosclerosis (hearing loss caused by changes to the bones in your ear)
have very high levels of fat in your blood (triglycerides)
have fluid retention due to heart or kidney problems
have a condition where your thyroid gland fails to produce enough thyroid hormone
(hypothyroidism) and you are treated with thyroid hormone replacement therapy
have a hereditary condition causing recurrent episodes of severe swelling (hereditary
angioedema) or if you have had episodes of rapid swelling of the hands, face, feet,
lips, eyes, tongue, throat (airway blockage) or digestive tract
have a lactose intolerance
have any other medical conditions
take any medicines for any other condition.
Cancer risk
Endometrial hyperplasia and cancer
Taking estrogen-only HRT will increase the risk of excessive thickening of the lining
of the uterus (endometrial hyperplasia) and cancer of the uterus lining (endometrial
cancer).
The progestogen in Trisequens® reduces this extra risk.
In women who still have a uterus and who are not taking HRT, on average, 5 in 1,000
will be diagnosed with endometrial cancer between the ages of 50 and 65.
For women aged 50 to 65 who still have a uterus and who take estrogen-only HRT, between
10 and 60 women in 1,000 will be diagnosed with endometrial cancer, depending on the
dose and for how long it is taken.
Irregular bleeding
You may have irregular bleeding or drops of blood (spotting) during the first 3-6
months of taking Trisequens®. However, see your doctor as soon as possible if the
irregular bleeding:
carries on for more than 6 months
starts after you have been taking Trisequens® for more than 6 months
carries on after you have stopped taking Trisequens®.
Breast cancer
Evidence shows that taking combined estrogen-progestogen or estrogen-only HRT increases
the risk of breast cancer. The extra risk depends on how long you use HRT. The additional
risk becomes clear within 3 years of use. After stopping HRT the extra risk will decrease
with time, but the risk may persist for 10 years or more if you have used HRT for
more than 5 years.
Risk with 5 years of use
For women aged 50 who start taking estrogen-progestogen HRT for 5 years, it is estimated
that 21 cases of breast cancer in 1000 users are diagnosed, compared with 13 to 17
cases per 1000 in those who do not take HRT.
Risk with 10 years of use
For women aged 50 who start taking estrogen-progestogen HRT for 10 years, it is estimated
at 48 cases of breast cancer in 1,000 users are diagnosed, compared with 27 cases
per 1,000 in those who did not take HRT.
Ovarian cancer
Ovarian cancer is rare – much rarer than breast cancer. The use of estrogen-only or
combined estrogen-progestogen HRT has been associated with a slightly increased risk
of ovarian cancer.
Blood clots in a vein (venous thromboembolism)
The risk of blood clots in the veins is about 1.3 to 3 times higher in HRT users than
in non-users, especially during the first year of taking it.
Blood clots can be serious, and if one travels to the lungs, it can cause chest pain,
breathlessness, fainting or even death.
Inform your doctor if any of these risks apply to you:
you are unable to walk for a long time because of major surgery, injury or illness
you have had one or more miscarriages
you are overweight or obese (BMI >30 kg/m²)
you have any blood clotting problem that needs long-term treatment with a medicine
used to prevent blood clots
if any of your close relatives has ever had a blood clot in the leg, lung or another
organ
you have systemic lupus erythematosus (SLE)
you have cancer.
Heart disease (heart attack)
There is no evidence that HRT will prevent a heart attack. Women over the age of 60
years who use estrogen-progestogen HRT are slightly more likely to develop heart disease
than those not taking any HRT.
Stroke
The risk of having as stroke is about 1.5 times higher in HRT users than in non-users.
The number of extra cases of stroke due to use of HRT will increase with age.
Other things that can increase the risk of stroke include:
high blood pressure
smoking
drinking too much alcohol
an irregular heartbeat.
Other conditions
HRT will not prevent memory loss. There is some evidence of a higher risk of memory
loss in women who start using HRT after the age of 65.
Tell your doctor or the laboratory staff that you are taking Trisequens® if you need
a blood test. This is because this medicine can affect the results of some tests.
During treatment, you may be at risk of developing certain side effects. It is important
you understand these risks and how to monitor for them. See additional information
under Section
6. Are there any side effects?
Pregnancy and breastfeeding
Do not take Trisequens® if you are pregnant or suspect you are pregnant.
Do not take Trisequens® if you are breastfeeding.
3. What if I am taking other medicines?
Tell your doctor or pharmacist if you are taking any other medicines, including any
medicines, vitamins or supplements that you buy without a prescription from your pharmacy,
supermarket or health food shop.
Some medicines may interfere with Trisequens® and affect how it works; Trisequens®
may interfere with some medicines and affect how they work.
Medicines that may
increase
the effect of Trisequens® include:
other medicines containing estrogens
some anti-infectives, e.g. ketoconazole
Medicines that may
reduce
the effect of Trisequens® include:
medicines to help you sleep, including barbiturates
medicines for epilepsy e.g. phenytoin, carbamazepine, lamotrigine
some antibiotics and other anti-infective medicines, e.g. - rifampicin, rifabutin,
nevirapine, efavirenz, ritonavir, telaprevir and nelfinavir
medicines for hepatitis C infections, e.g. telaprevir
St John's Wort - used to treat depression, low mood
antihistamines - used to treat allergies
Trisequens® may
increase
the effectiveness of some medicines. These include:
corticosteroids - used to treat inflammatory conditions
Imipramine
pethidine
cyclosporin
Trisequens® may
reduce
the effectiveness of some medicines. These include:
lamotrigine - a medicine to treat epilepsy
some medicines used to treat depression
blood thinners used to prevent clots
medicines used to treat diabetes
thyroid hormones - used to treat poorly functioning thyroid gland.
Check with your doctor or pharmacist if you are not sure about what medicines, vitamins
or supplements you are taking and if these affect Trisequens®.
4. How do I use Trisequens®?
How much to take
Carefully read the instructions below, in order to correctly use the calendar pack.
Take one tablet a day, preferably at the same time each day, until all 28 tablets
have been taken.
Days 1–12:
Take one blue tablet every day for 12 days.
Days 13–22:
Take one white tablet every day for 10 days.
Days 23–28:
Take one red tablet every day for 6 days.
Swallow each tablet with a glass of water. When you have finished each pack, start
the next pack immediately.
When to take Trisequens®
Your doctor will tell you when to start taking the tablets.
If you are still having periods, you would usually take the first tablet on the fifth
day after the start of your period.
If your periods have stopped or have become infrequent, the first tablet can be taken
as soon as you get the product.
How to use the calendar pack
1. Set the day reminder
Turn the inner disk to set the day of the week opposite the little plastic tab.

2. Take the first day’s tablet
Break the plastic tab and tip out the first tablet.
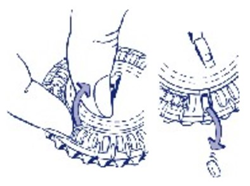
3. Move the dial every day
On the next day simply move the transparent dial clockwise one space as indicated
by the arrow. Tip out the next tablet. Remember to take only one tablet once a day.
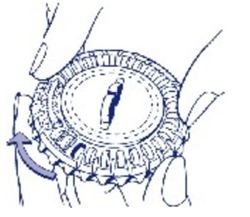
You can only turn the transparent dial after the tablet in the opening has been removed.
If you forget to use Trisequens®
You can always see if you have taken your tablet by looking at the day on the calendar
pack.
If you forget to take a tablet at the usual time, throw away the tablet you missed
and take your next dose when you are meant to.
Do not take a double dose to make up for the dose you missed.
You may have vaginal bleeding or spotting if you forget to take your tablets.
If you take too much Trisequens®
If you think that you or anyone else may have taken too many Trisequens® tablets you
may need medical attention.
You should:
phone the Poisons Information Centre
(by calling
13 11 26), or
contact your doctor, or
go to the Emergency Department at your nearest hospital.
You should do this even if there are no signs of discomfort or poisoning.
5. What should I know while using Trisequens®?
Things you should do
Regularly check your breasts
See your doctor if you notice changes, such as:
dimpling of the skin
changes to the nipple
any lumps you can feel.
Go for regular breast screening and pap smear tests.
Once you've started on HRT, you should see your doctor for regular check-ups (at least
once a year). At these check-ups, your doctor may discuss with you the benefits and
risks of continuing to take HRT.
If you need to have surgery, tell your surgeon you are taking HRT, and specifically
Trisequens®. You may need to stop taking your tablets a few weeks prior to your surgery.
If you have stopped therapy, ask your doctor when you can start taking Trisequens®
again.
Call your doctor straight away if you:
Become pregnant while taking Trisequens®. Trisequens® is for use in postmenopausal
women, only.
Remind any doctor, dentist or pharmacist you visit that you are taking Trisequens®.
Things you should not do
Do not stop using this medicine suddenly.
Do not change the way you are taking Trisequens®
Do not give Trisequens® to anyone else, even if you think they may have the same condition
as you.
Do not take Trisequens® if you are breastfeeding.
Driving or using machines
Be careful before you drive or use any machines or tools until you know how Trisequens®
affects you.
Drinking alcohol
Tell your doctor if you drink alcohol.
Looking after your medicine
Follow the instructions in the carton on how to take care of your medicine properly.
Store it in a cool dry place away from moisture, heat or sunlight; for example, do
not store it:
in the bathroom or near a sink, or
in the car or on window sills.
Keep the calendar pack in the outer carton in order to protect from light.
Do not put Trisequens® in the refrigerator.
Keep it where young children cannot reach it.
When to discard your medicine
Discard all medicine if it is after the expiry date printed on the pack. The expiry
date refers to the last day of that month.
Do not use your medicine if the packaging is torn or shows signs of tampering.
Getting rid of any unwanted medicine
If you no longer need to use this medicine or it is out of date, take it to any pharmacy
for safe disposal.
Do not use this medicine after the expiry date.
6. Are there any side effects?
All medicines can have side effects. If you do experience any side effects, most of
them are minor and temporary. However, some side effects may need medical attention.
When you start taking Trisequens® your body has to adjust to new hormone levels. See
the information below and, if you need to, ask your doctor or pharmacist if you have
any further questions about side effects.
Less serious side effects
Serious side effects
Tell your doctor or pharmacist if you notice anything else that may be making you
feel unwell.
Other side effects not listed here may occur in some people.
Reporting side effects
After you have received medical advice for any side effects you experience, you can
report side effects to the Therapeutic Goods Administration online at
www.tga.gov.au/reporting-problems . By reporting side effects, you can help provide more information on the safety of
this medicine.
Always make sure you speak to your doctor or pharmacist before you decide to stop
taking any of your medicines.
7. Product details
This medicine is only available with a doctor's prescription.
What Trisequens® contains
| Each red tablet contains: |
|
Active ingredient
(main ingredient)
|
1 mg estradiol hemihydrate
|
|
Other ingredients
(inactive ingredients)
|
lactose monohydrate
maize starch
purified talc
magnesium stearate
hyprolose
hypromellose
titanium dioxide (E171)
propylene glycol
iron oxide red CI77491 (E172)
|
|
Potential allergens
|
lactose monohydrate
|
| Each blue tablet contains: |
|
Active ingredient
(main ingredient)
|
2 mg estradiol hemihydrate
|
|
Other ingredients
(inactive ingredients)
|
lactose monohydrate
maize starch
purified talc
magnesium stearate
hyprolose
hypromellose
titanium dioxide (E171)
macrogol 400
indigo carmine CI73015 (E132)
|
|
Potential allergens
|
lactose monohydrate
|
| Each white tablet contains: |
|
Active ingredient
(main ingredient)
|
2 mg estradiol hemihydrate
1 mg norethisterone acetate
|
|
Other ingredients
(inactive ingredients)
|
lactose monohydrate
maize starch
purified talc
magnesium stearate
hyprolose
hypromellose
triacetin
|
|
Potential allergens
|
lactose monohydrate
|
Do not take this medicine if you are allergic to any of these ingredients.
What Trisequens® looks like
Trisequens® comes in a calendar dial pack. Each pack holds 28 tablets.
Trisequens® calendar dial pack contains:
12 blue film-coated, biconvex tablets engraved with 'NOVO 280'.
10 white film-coated, biconvex tablets engraved with 'NOVO 281'.
6 red film-coated, biconvex tablets engraved with 'NOVO 282'.
AUST R 192476
Who distributes Trisequens®
Novo Nordisk Pharmaceuticals Pty Ltd
Level 10
118 Mount Street
North Sydney NSW 2060
Australia
Trisequens® is registered trademark of Novo Nordisk Health Care AG.
© 2025
Novo Nordisk A/S
Further information
For further information call Novo Nordisk Medical Information on 1800 668 626.
Always check the following websites to ensure you are reading the most recent version
of the Consumer Medicine Information:
This leaflet was prepared in December 2025.