Introduction
What are bacteriophages?
History and revival
Phages and the gut microbiome
Therapeutic potential
Challenges
References
Further reading
Phage therapy is an emerging strategy that uses viruses that target bacteria to restore gut balance and treat microbiome-related diseases. Ongoing research and early trials show promise, but regulatory, manufacturing, and precision-matching challenges still limit widespread clinical use.
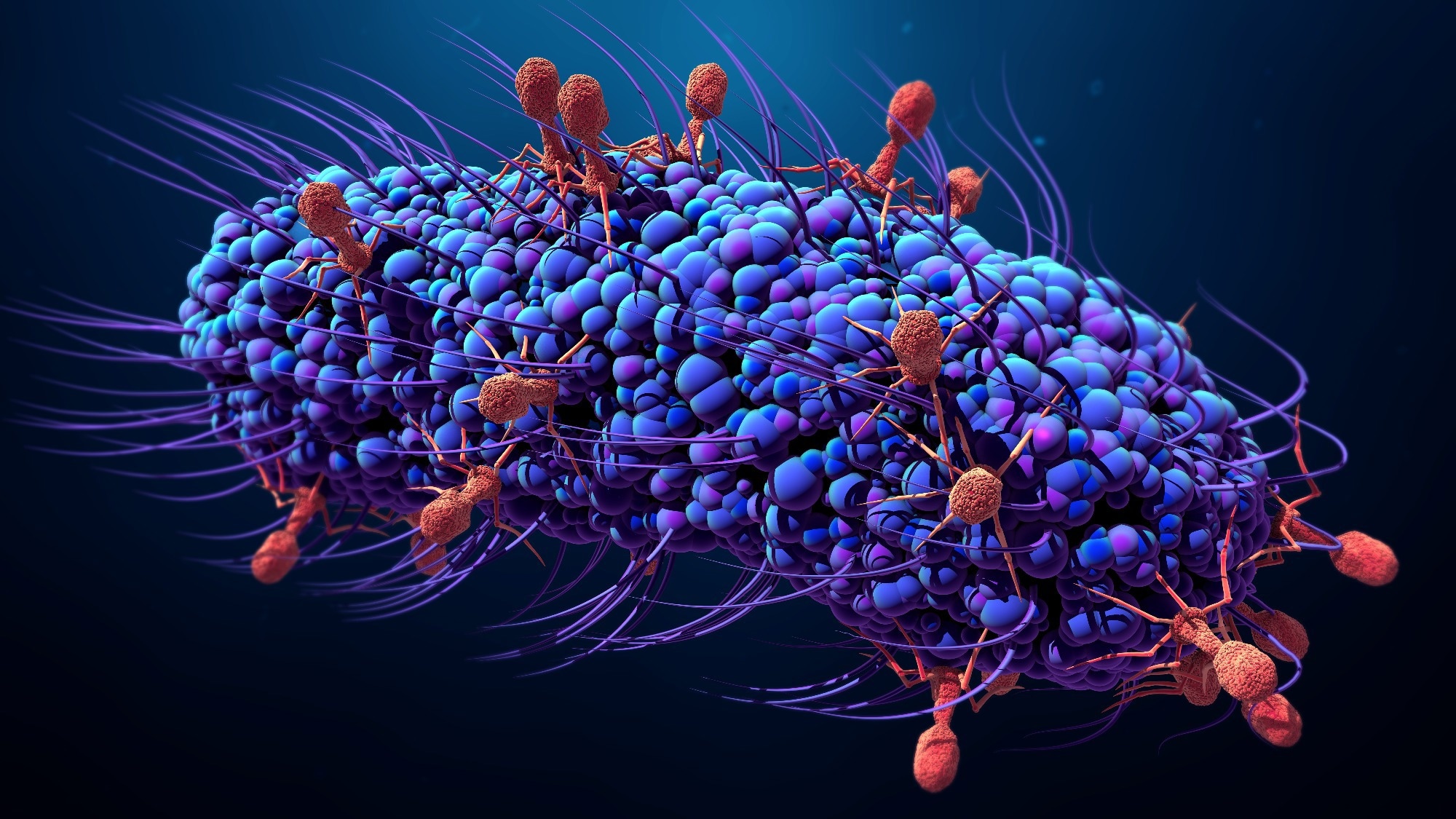 Image Credit: Design_Cells / Shutterstock.com
Image Credit: Design_Cells / Shutterstock.com
Introduction
As insights into host-microbiota interactions expand, phage therapy has emerged as a promising next-generation approach for restoring gut homeostasis and treating microbiome-associated diseases.1,2,5
What are bacteriophages?
Bacteriophages are viruses that infect and kill bacteria with remarkable specificity, as each phage typically targets only one bacterial species or particular strain. Bacteriophages are the most abundant biological entities present on Earth, with an estimated 10³¹ particles present globally, thus forming an integral part of the human virome and broader biosphere.3
Bacteriophages attach to a bacterial cell and subsequently inject their genetic material to produce new viral copies within the cell. The infected bacterium eventually lyses, which leads to the release of new phages that infect neighboring bacterial cells.2
Only lytic bacteriophages are currently used in clinical phage therapy, because they kill bacteria without integrating into the host genome.2,4,6,10 Specialized enzymes, such as holins and endolysins, destroy bacterial membranes and cell walls to ensure rapid bacterial death and phage release. These mechanisms allow phages to target antibiotic-sensitive and antibiotic-resistant bacteria while minimizing disruption to beneficial microorganisms.4
In addition to natural variants, researchers are now engineering phages to enhance their specificity and potency. Engineered phages can be programmed to alter bacterial gene expression, broaden host range, or deliver therapeutic molecules, thus offering a novel approach for combating resistant infections and restoring microbial balance in the gut.4,5,10,18
History and revival
Bacteriophages were first identified in 1915 by British pathologist Frederick Twort and later characterized by Félix d'Hérelle in 1917, who recognized their ability to infect and destroy bacteria. In 1921, d'Hérelle conducted one of the first successful human trials using phages to treat dysentery decades before antibiotics became available.2,6
Following the discovery of penicillin in the 1930s, interest in phage therapy declined in Western medicine, while research continued in Eastern Europe and the former Soviet Union.3,5,6 However, the growing global crisis of antibiotic resistance has revived scientific and clinical interest in phage therapy as a precise and adaptive antimicrobial strategy that selectively eliminates harmful bacteria while preserving commensal species.4,6
Compassionate-use reports indicate notable success in treating Pseudomonas aeruginosa lung infections in cystic fibrosis patients and Staphylococcus aureus prosthetic joint infections, wherein phage formulations have achieved significant reductions in bacterial burden and symptom improvement.7 Systematic reviews summarizing these modern case series and early trials suggest that a clear majority of treated patients experience clinical improvement and microbiological response, although most data still derive from uncontrolled or compassionate-use settings.7,8
The Deadliest Being on Planet Earth – The Bacteriophage
Phages and the gut microbiome
Bacteriophages are natural residents of the human intestine and collectively form the gut phageome, a crucial regulator of microbial community structure and balance. By selectively infecting and lysing specific bacterial hosts, phages can help maintain intestinal homeostasis and may limit the overgrowth of pathogenic species such as Clostridioides difficile and Escherichia coli.2,6
The crAssphage genus, one of the most abundant viral groups in the human gut, is present in over 50% of individuals and can account for up to 90% of total viral deoxyribonucleic acid (DNA) in stool. Phages can modulate dysbiosis, a microbial imbalance associated with inflammatory bowel diseases (IBDs) like Crohn’s disease and ulcerative colitis, by reducing pathogenic bacteria and promoting eubiosis.6
Preclinical and early human studies highlight the therapeutic potential of bacteriophages, with sterile, virus-enriched fecal filtrates (fecal filtering transplants) reported to resolve recurrent C. difficile infection and normalize stool habits in small patient series.1,6 In murine models, phage formulations targeting adherent-invasive E. coli (AIEC) reduced intestinal bacterial load and colitis severity, while other studies have reported phage-mediated alleviation of steatohepatitis and metabolic syndrome.6,10,11
In one study using the PDX phage, a member of the Myoviridae family, effective lysis of diarrheagenic, enteroaggregative E. coli was observed both in vitro and in a murine intestinal colonization model. A single oral dose of PDX significantly reduced E. coli colony counts for several days after infection without measurably altering alpha or beta diversity in the surrounding microbiota.6,9
Emerging evidence suggests that phages can subtly shift gut communities toward butyrate-producing bacteria and may modestly influence mucosal immune markers, such as circulating interleukin-4, without globally disrupting community structure. By fermenting dietary fiber, these bacteria produce butyrate, a key source of energy for colon cells and a vital factor in maintaining gut health.2,12,14,17
Therapeutic potential
Recent clinical and preclinical studies highlight advances in personalized phage therapy, synergistic combinations, and engineered phage systems that could be used as alternatives to conventional antibiotics.2,4,5,6,18 Personalized approaches remain essential, as limited efficacy often reflects poor host-phage matching.6,7,8
For example, a prospective randomized clinical trial tested an oral cocktail of eleven T4-like coliphages in children with acute diarrhea. Despite no clinical improvement, the treatment was well tolerated, confirming the safety of phage in intestinal transit.13
Similar findings have been reported in adults with mild gastrointestinal distress treated with a four-phage cocktail containing LH01-Myoviridae, LL5-Siphoviridae, T4D-Myoviridae, and LL12-Myoviridae, which safely reduced E. coli loads and produced a small but significant decrease in circulating interleukin-4, without significantly altering global alpha or beta diversity.14
Combining phages with probiotics and prebiotics enhances therapeutic outcomes. Co-administration of phages with E. coli Nissle-1917 in murine models achieved over a three-log reduction in multidrug-resistant E. coli colonization, while preserving microbial balance.16 Similar synergy has been observed in dietary supplements and animal studies promoting gut health and infection prevention.12,17
Building on preclinical work in AIEC-driven inflammation, a phase 2 double-blind, placebo-controlled trial (EcoActive) is currently evaluating an oral AIEC-targeting phage cocktail in patients with inactive Crohn’s disease (ClinicalTrials.gov NCT03808103).6,11,15
Beyond direct therapy in the gut, bacteriophages are also being incorporated into food safety strategies to reduce contamination by food-borne pathogens such as Salmonella and Listeria, potentially lowering the infectious burden that reaches the intestinal tract.3,19
Meanwhile, synthetic biology is enabling the creation of stable, programmable phages. Engineered systems, such as clustered regularly interspaced short palindromic repeats (CRISPR) associated protein (Cas)-armed phage cocktail SNIPR001, selectively target intestinal E. coli and reduce the emergence of phage-tolerant or antibiotic-resistant subpopulations in preclinical models.10,18
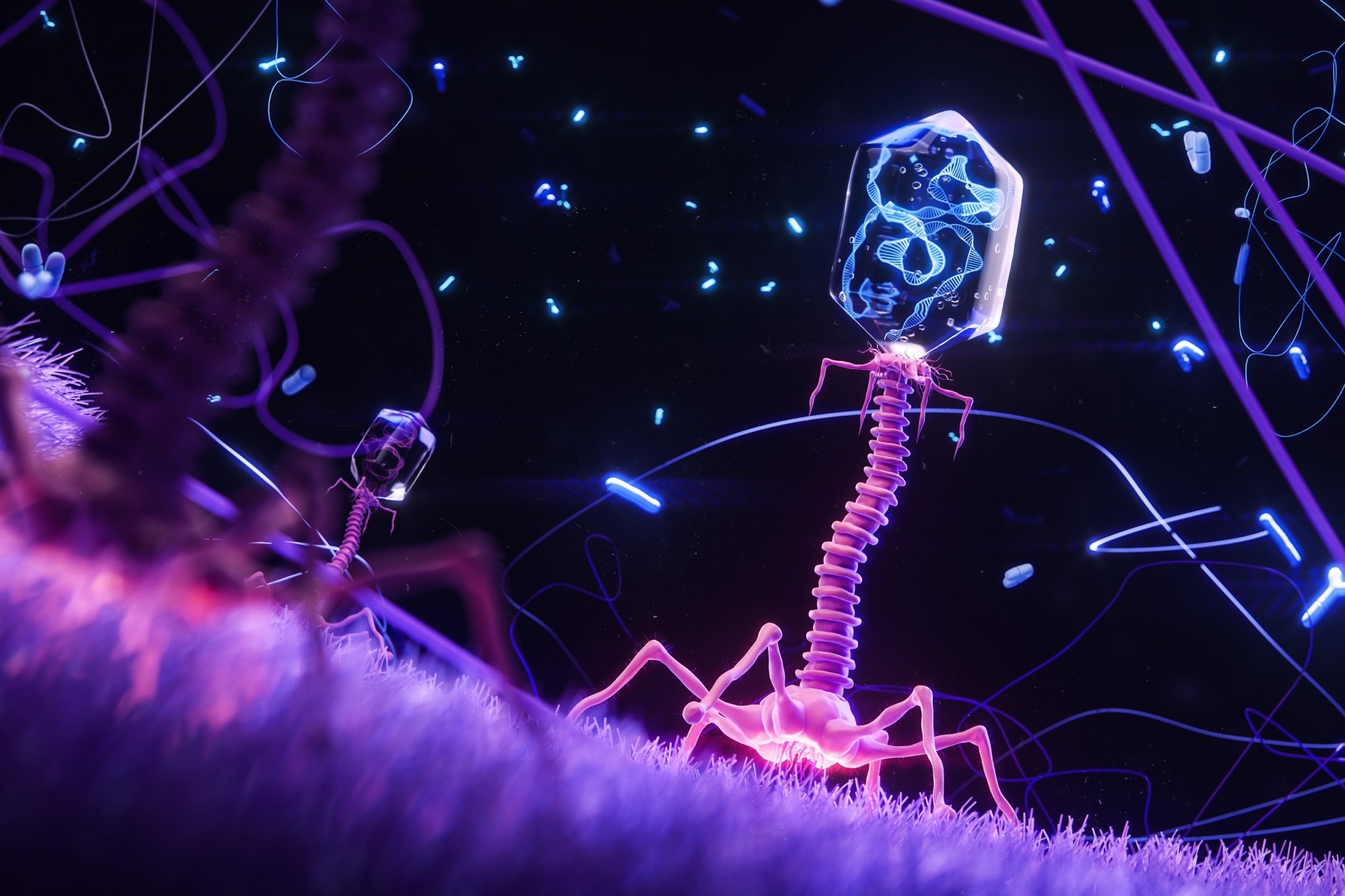 Image Credit: KateStudio / Shutterstock.com
Image Credit: KateStudio / Shutterstock.com
Challenges
The United States Food and Drug Administration (FDA) classifies bacteriophages as Investigational New Drugs (IND) with single-patient or compassionate-use approvals for severe or antibiotic-resistant infections when standard treatments have failed. Although early clinical studies have demonstrated safety, regulatory agencies like the FDA require robust, large-scale trial data and validated production protocols to establish consistent efficacy and manufacturing quality.2,5,7,8
Unlike antibiotics, which are chemically defined and mass-produced, phages are biological entities that evolve with their bacterial hosts. The high specificity of bacteriophages means that even closely related bacterial strains require distinct phage preparations, underscoring the importance of consistent isolation, purification, genomic characterization, and potency testing.
Establishing uniform Good Manufacturing Practice (GMP) standards for phage production, including stable formulation, storage, and quality control, remains complex. Differences in host bacteria used for propagation can influence phage yield and purity, while endotoxin contamination during bacterial lysis poses additional safety concerns.5
Bacteria can acquire resistance to phages through spontaneous mutations, restriction–modification systems, or CRISPR-Cas immunity. As a result, engineered phages are associated with potential biosafety concerns, including horizontal gene transfer or unforeseen impacts on microbial communities. Continued genomic and ecological surveillance will be crucial to mitigate these risks.4,5,10,18
Despite these limitations, ongoing research in synthetic biology, phage engineering, and controlled clinical trials across the U.S. and Europe is addressing these barriers. Regulatory frameworks are beginning to adapt, signaling cautious optimism that phage therapy could soon complement antibiotic strategies in precision infection control.1,2,5,7,8,15
References
- Manrique, P., Montero, I., Fernandez-Gosende, M., et al. (2024). Past, present, and future of microbiome-based therapies. Microbiome Research Reports 3(2); 23. DOI:10.20517/mrr.2023.80, https://www.oaepublish.com/articles/mrr.2023.80.
- Paule, A., Frezza, D., & Edeas, M. (2018). Microbiota and Phage Therapy: Future Challenges in Medicine. Medical Sciences 6(4); 86. DOI:10.3390/medsci6040086, https://www.mdpi.com/2076-3271/6/4/86.
- AL-Ishaq, R. K., Skariah, S., & Büsselberg, D. (2020). Bacteriophage Treatment: Critical Evaluation of Its Application on World Health Organization Priority Pathogens. Viruses 13(1); 51. DOI:10.3390/v13010051, https://www.mdpi.com/1999-4915/13/1/51.
- Hibstu, Z., Belew, H., Akelew, Y., & Mengist, H. M. (2022). Phage Therapy: A Different Approach to Fight Bacterial Infections. Biologics: Targets & Therapy 16; 173. DOI:10.2147/BTT.S381237, https://www.dovepress.com/phage-therapy-a-different-approach-to-fight-bacterial-infections-peer-reviewed-fulltext-article-BTT.
- Alsayed, A. R., & Permana A., D. (2024). Bacteriophages Therapy: Exploring Their Promising Role in Microbiome Modulation and Combating Antibiotic Resistance. OBM Genetics 8(2):237. DOI:10.21926/obm.genet.2402237, https://www.lidsen.com/journals/genetics/genetics-08-02-237.
- Gutiérrez, B., & Domingo-Calap, P. (2020). Phage Therapy in Gastrointestinal Diseases. Microorganisms 8(9); 1420. DOI:10.3390/microorganisms8091420, https://www.mdpi.com/2076-2607/8/9/1420.
- Abedon, S. T., Danis-Wlodarczyk, K. M., & Alves, D. R. (2021). Phage Therapy in the 21st Century: Is There Modern, Clinical Evidence of Phage-Mediated Efficacy? Pharmaceuticals 14(11); 1157. DOI:10.3390/ph14111157, https://www.mdpi.com/1424-8247/14/11/1157.
- Uyttebroek, S., Chen, B., Onsea, J., et al. (2022). Safety and efficacy of phage therapy in difficult-to-treat infections: a systematic review. Lancet Infect Diseases 22(8); e208–e220. DOI:10.1016/S1473-3099(21)00612-5, https://www.thelancet.com/journals/laninf/article/PIIS1473-3099(21)00612-5/abstract.
- Cepko, L. C. S., Garling, E. E., Dinsdale, M. J., et al. (2020). Myoviridae phage PDX kills enteroaggregative Escherichia coli without human microbiome dysbiosis. Journal of Medical Microbiology 69(2); 309–323. DOI:10.1099/jmm.0.001162, https://www.microbiologyresearch.org/content/journal/jmm/10.1099/jmm.0.001162,
- Monteiro, R., Pires, D. P., Costa, A. R., & Azeredo, J. (2019). Phage Therapy: Going Temperate? Trends in Microbiology 27(4); 368–378. DOI:10.1016/j.tim.2018.10.008, https://www.cell.com/trends/microbiology/abstract/S0966-842X(18)30231-2.
- Galtier, M., De Sordi, L., Sivignon, A., et al. (2017). Bacteriophages Targeting Adherent Invasive Escherichia coli Strains as a Promising New Treatment for Crohn's Disease. Journal of Crohn’s and Colitis 11(7); 840–847. DOI:10.1093/ecco-jcc/jjw224, https://academic.oup.com/ecco-jcc/article-abstract/11/7/840/2895107.
- Kiani, A. K., Anpilogov, K., Dautaj, A., et al. (2020). Bacteriophages in food supplements obtained from natural sources. Acta Bio Medica: Atenei Parmensis 91(Suppl 13); e2020025. DOI:10.23750/abm.v91i13-S.10834, https://www.mattioli1885journals.com/index.php/actabiomedica/article/view/10834.
- Sarker, S. A., Sultana, S., Reuteler, G., et al. (2016). Oral Phage Therapy of Acute Bacterial Diarrhea With Two Coliphage Preparations: A Randomized Trial in Children From Bangladesh. eBioMedicine 4; 124–37. DOI:10.1016/j.ebiom.2015.12.023, https://www.thelancet.com/journals/ebiom/article/PIIS2352-3964(15)30251-6/fulltext.
- Febvre, H. P., Rao, S., Gindin, M., et al. (2019). PHAGE Study: Effects of Supplemental Bacteriophage Intake on Inflammation and Gut Microbiota in Healthy Adults. Nutrients 11(3):666. DOI:10.3390/nu11030666, https://www.mdpi.com/2072-6643/11/3/666.
- Intralytix, Inc. (2025, June 15). Safety and Efficacy of EcoActive on Intestinal Adherent Invasive E. Coli in Patients With Inactive Crohn's Disease (NCT03808103). ClinicalTrials.gov., https://www.clinicaltrials.gov/study/NCT03808103. Accessed on 5 November 2025
- Porter, S. B., Johnston, B. D., Kisiela, D., et al. (2022). Bacteriophage Cocktail and Microcin-Producing Probiotic Escherichia coli Protect Mice Against Gut Colonization with Multidrug-Resistant Escherichia coli Sequence Type 131. Frontiers in Microbiology 13. DOI:10.3389/fmicb.2022.887799, https://www.frontiersin.org/journals/microbiology/articles/10.3389/fmicb.2022.887799/full.
- Shaufi, M. A. M., Sieo, C. C., Chong, C. W., et al. (2022). Effects of Phage Cocktail, Probiotics, and Their Combination on Growth Performance and Gut Microbiota of Broiler Chickens. Animals 13(8); 1328. DOI:10.3390/ani13081328, https://www.mdpi.com/2076-2615/13/8/1328.
- Gencay, Y. E., Jasinskyte, D., Robert, C., et al. (2023). Engineered phage with antibacterial CRISPR–Cas selectively reduces E. Coli burden in mice. Nature Biotechnology 42(2); 265. DOI:10.1038/s41587-023-01759-y, https://www.nature.com/articles/s41587-023-01759-y.
- Deepa, G., Daniel, I., & Sugumar, S. (2025). An insight into the applications of bacteriophages against food-borne pathogens. Journal of Food Science and Technology 62; 1–10. DOI:10.1007/s13197-024-06070-5, https://link.springer.com/article/10.1007/s13197-024-06070-5.
Last Updated: Nov 20, 2025