Skip to:
Cervical spondylosis is a degenerative disease that affects the spinal disks in the neck. It is a very common condition affecting more than 80% of the population over the age of 60 years.
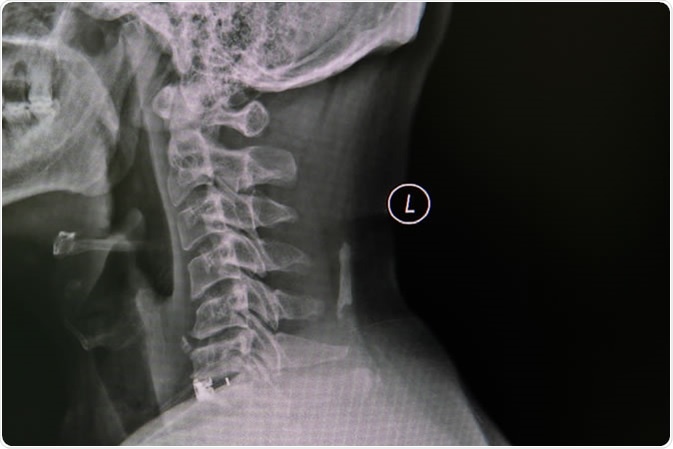
Cervical Spine, spinal cord and spondylosis, impressions with narrowing of the C5 / 6 area - Image Credit: nuiza11 / Shutterstock
What is cervical spondylosis?
Cervical spondylosis (CS) is a medical condition used to define age-related wears and tears of the spine. It mainly occurs in the cervical spine, which consists of seven small spinal bones (vertebrae) that form the neck.
The condition is mostly asymptomatic; however, degenerative spinal changes sometimes compress the nerve fibers that run through the spinal canal, leading to weakness or numbness in the legs, arms, and hands.
What are the causes of cervical spondylosis?
Anatomically, the spine is composed of 24 small bones (vertebrae) that form the spinal canal. Intervertebral discs are present in between the bones to provide a cushioning effect. With age, degenerative changes in the spine cause compression of the disks. They also become dehydrated and weak over time. All these changes ultimately result in collapsing of the disk space and loss of disk space height.
As a result, pressure on the spine joints (facet joints) increases, and the cartilage that covers the joints breaks down, leading to development of the signs of osteoarthritis.
A complete loss of cartilage can result in bone to bone friction and development of new bony overgrowth called bone spurs. These spurs can compress the nerve fibers in the spinal canal, leading to development of spinal stenosis.
Sometimes, cracks also appear on the disks, making them bulged. The bulged disks (herniated disks) can also compress the spinal cord or the nerve fibers.
In CS, loss of neck flexibility can occur due to hardening of the spinal ligaments with age.
Cervical Spondylosis. Symptoms
What are the symptoms of cervical spondylosis?
The most common symptoms of CS are mild to severe pain and stiffness in the neck. The intensity of the symptoms increases when the neck is held in a particular position for a long time, such as during driving a car or reading a book. The neck pain often spreads to the arms or shoulders.
The pain experienced in CS may become worse in certain conditions, such as after standing or sitting; during sneezing, coughing, or laughing; and at night.
A grinding noise or sensation may occur while moving the neck. Moreover, compression of the spinal cord or nerve fibers can lead to weakness or numbness in the arms, hands, legs, and fingers. The nerve compression may also cause lack of coordination and balance during movement of the body.
Some people experience headaches, especially at the backside of the head, and loss of bladder or bowel control.
What are the risk factors?
The most common risk factor for CS is age. The condition is very much associated with the normal age-related changes in the body.
Some people inherit the tendency to develop CS. A family history of neck pain is often a contributing factor.
A previous incidence of neck injury or spinal surgery can sometimes increase the chance of developing CS. Moreover, emotional distress, such as depression and anxiety, can be a risk factor.
Occupations that demand putting extra stress on the neck, such as those with a lot of repetitive neck movements, awkward positioning of the neck, or excessive overhead work, can make people more susceptible to CS.
Among lifestyle factors, smoking is known to significantly increase the risk of CS. In addition, being physically inactive or being overweight can also contribute.
People with severe arthritis in other body areas are also likely to develop CS.
What are the complications?
In some very rare cases, permanent damage or disability can occur due to too much compression of the spinal cord or nerve fibers.
A person with CS should immediately seek medical attention if he/she experiences sudden loss of movement; sudden feeling of weakness or numbness; or loss of bladder or bowel control.
Further Reading
Last Updated: Oct 6, 2019