Several decellularized materials have recently been synthesized that have previously demonstrated significant potential in the treatment of cardiovascular diseases, therefore improving the understanding of cardiac muscle growth.
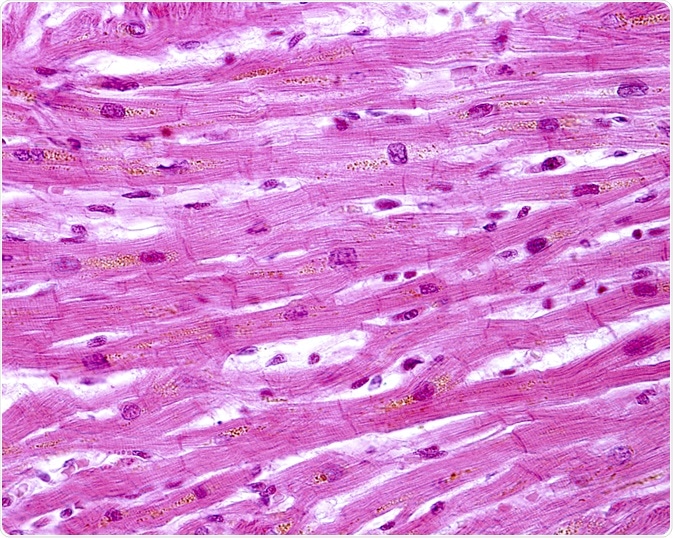 Image Credits: Jose Luis Calvo / Shutterstock.com
Image Credits: Jose Luis Calvo / Shutterstock.com
Out of these new biomaterials, decellularized myocardial matrix hydrogels have recently shown great potential for synthesizing cellular microenvironments that are representative of naturally occurring cardiac tissue, and therefore are able to successfully treat the heart after a heart attack.
These specific hydrogels, which originally derive from porcine cardiac tissue, eventually form a nano-fibrous hydrogel when they are thermally induced at mammalian body temperatures (approximately 37°C). The persistent use of this isolated cardiac matrix in both 2-dimensional and 3-dimensional in vitro settings has shown the potential to give tissue-specific instructions for cardiac muscle cell differentiation and growth.
How are decellularized myocardial matrix hydrogels used?
Scientific testing of myocardial matrix hydrogels as an option for therapy post-myocardial infarction that was done in both large and small mammalian models has consistently shown increased cardiac muscle and improved left ventricular function, as well as cellular recruitment into the damaged regions of the heart. Therefore, based upon those results, additional steps are now being taken to make use of this new hydrogel technology as an injectable biomaterial treatment for human heart attack patients.
Significant progress in cardiac tissue bio-engineering has shown great potential in the long-term pursuit of corrective treatment of cardiovascular diseases, such as a heart attack. Ischemic heart disease, which can ultimately lead to myocardial infarction (MI) as well as subsequent heart failure, is the most common cause of death not only in the western world but throughout the globe, with an increase of up to 13.4% of overall annual deaths projected worldwide by the year 2030.
After experiencing an MI the adult human heart does not have the regenerative capacity to repair any damaged cells, leading onto some progressive biological cell remodeling, such as the degradation of extracellular matrices performed by matrix metalloproteinases.
Prevention of heart failure post-myocardial infarction
Currently, there are no other treatments available that are capable of preventing a heart failure post-myocardial infarction, with the treatment options for late-stage heart failure being limited to left ventricular assistance devices, or whole heart transplant. Unfortunately, these treatment options tend to put a heavy strain upon patients' quality of life, and also require a range of expensive medical resources.
As a response to this situation, scientific research into cardiac tissue bioengineering is currently focusing on the investigation into whether the restoration of function and potential full/partial regeneration of any damaged heart cells, could possibly be achieved using novel methods of treatment.
Isolation of the extracellular matrix
Recent advancement in myocardial bioengineering that has significantly accelerated heart disease research is the successful isolation of underlying extracellular matrix scaffolding from naturally formed cardiac tissue.
The extracellular matrix within the heart provides the damaged cells with tissue-specific biochemical instructions, which have subsequently been demonstrated to be essential for cellular development, differentiation, and natural migration.
Promising studies
Studies performed after that discovery initially showed that decellularized porcine cardiac tissue can be bioengineered into an injectable biomaterial treatment that synthesizes a nano-fibrous porcine myocardial matrix hydrogel once placed into the body.
There have been further scientific studies, with the purpose being primarily to quantitatively analyze and identify when human cardiac extracellular matrix cells are isolated from several separate donor hearts. The extracellular matrix was firstly isolated via the decellularization of the six total human cadaveric donor hearts, which were then characterized by analyzing any sulfated glycosaminoglycan content.
The recorded protein content was then further evaluated. This study concluded that by using the appropriate analysis methods and quantifying the results, those human extracellular matrices can indeed be successfully characterized.
Conclusion
In conclusion, rigorous studies have proven that decellularized myocardial matrix hydrogels are a promising therapy for the treatment and recovery of patients that have previously suffered from myocardial infarction and/or heart failure.
This novel treatment could soon provide a viable and cheaper alternative to harsher options that are currently available, such as risky full-heart transplants that can take a long time to happen due to transplant lists, or enduring a surgery to insert a left ventricle assistance device that can significantly reduce the quality of a patient’s life. More research is required on live human patients, but this technology could be very beneficial to the medical community.
Sources
Wang R.M. & Christman K.L. (2016). Decellularized myocardial matrix hydrogels: In basic research and preclinical studies. https://doi.org/10.1016/j.addr.2015.06.002
Johnson T.D. et al. (2015). Quantification of decellularized human myocardial matrix: A comparison of six patients. https://doi.org/10.1002/prca.201500048
Further Reading
Last Updated: Mar 11, 2020