Jun 13 2018
Introduction
Phytochemicals are compounds produced by plants. They are emerging as potential new weapons of great power against resistant bacterial strains.
Antibiotics, are among the most important human discoveries of the 20th century, increasing the life expectancy dramatically as well as improving the quality of life worldwide. Antibiotic usage has led to the prevention of millions of deaths, and the global sale of antibiotics achieves almost 40 billion USD. However, with the soaring use of antibiotics, another monster has reared its head: antibiotic resistance. The answer to this could be extracting inexpensive antimicrobial products from plants, especially useful for developing countries.
Most antibiotics in current use are therefore derivatives of natural compounds. Natural antibiotics actually begin their history with the discovery of Penicillium chrysogenum-induced inhibition of bacterial growth around itself, by Alexander Fleming in 1928. It took several more years, but by the sixth and seventh decades of the 20th century, many antibiotic classes had developed from these natural antibiotics and entered clinical use.
These included the phenylpropanoids, glycopeptides, tetracyclines and macrolide antibiotics. After this there was a decline in the release of new antibiotic agents, with only four new classes of molecules having been brought on the market since then. None of these has made quite the impact that the earlier classes did. All subsequent antibiotics introduced into the market have been molecules based on the chemical alteration of these familiar structures.
Why is it so difficult to find new antibacterial molecules today? Partly, it is because of the general understanding that bacterial infection is no longer a mystery. This has been disproved by the exploding problem of antibiotic resistance posed by many bacteria that cause most common illnesses today. Even when antibiotic use is monitored and regulated by strict guidelines, bacterial resistance continues to mock the clinician and requires newer agents to combat this scourge. The emergence of pathogens which can defy even once the unconquerable antibiotics, has become a pressing problem which pushes researchers to find better answers.
These multidrug-resistant strains of bacterial pathogens are a lethal threat to humankind.
Antibiotic resistance
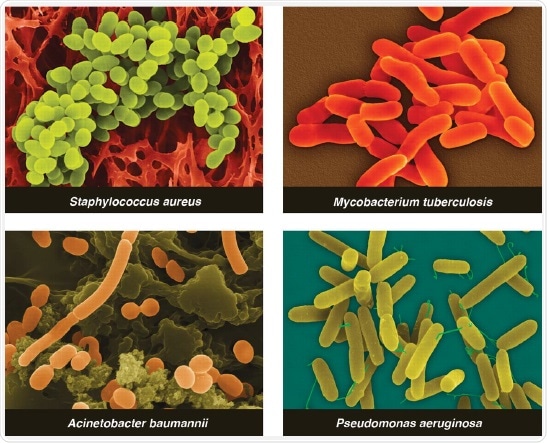
In public health today, the major challenges are posed by three antibiotic-resistant classes of disease-causing bacteria, shown above. The first is Staphylococcus aureus (MRSA), which causes at least 19,000 deaths per year and an annual addition of 4 billion USD to healthcare expenses in the US alone. It is sweeping into more and more regions, making it seem distinctly likely that S. aureus (VRSA) which is equally lethal, though even more difficult to treat than MRSA, will soon devastate hospitals.
The second type is multidrug-resistant (MDR) and pandrug-resistant (PDR) Gram-negative bacteria, which are fortunately less widespread at present, but are far more terrifying in that they cannot be treated with any known antibiotic. These include some strains of Escherichia coli, Pseudomonas aeruginosa, Acinetobacter baumannii, and Klebsiella pneumoniae. They defy either several or all commonly used antibiotics that are in use against Gram-negative bacteria.
It is unlikely that new antibiotics against these bacteria will be developed any time in the near future, because Gram-negative bacteria have outer cell membranes that prevent some antibiotics from entering, while they have efflux pumps that throw out many others.
The third category of resistant bacteria is composed of MDR and extensively drug-resistant (XDR) strains of Mycobacterium tuberculosis (MDR-TB and XDR-TB). These are becoming rampant in the developing world, because they must be treated for long periods and require much effort to oversee and monitor their treatment. The drugs used carry the risk of serious adverse effects which may even be fatal.
The result of this situation is a worldwide vulnerability to superbacteria which are seemingly invincible, posing the threat of severe disease outbreaks which will be almost impossible to treat. The only way out is to find and produce new antibiotics. Unlike other drug classes, today’s antibiotics are likely to be much less useful within decades or even years due to the increasing spread of these superbugs.
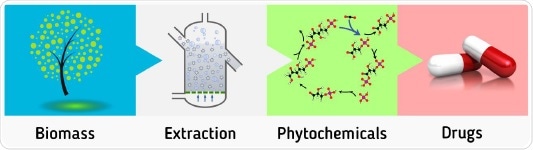
Phytochemicals: from source to medicine.
Phytochemicals
A study of plants in their environment shows that antibacterial products are part of the defenses set up by most plants as part of their metabolism, to keep themselves from succumbing to microbes, including a host of Gram-positive bacteria, around them. The soil in which plants grow is full of bacteria, fungi and viruses. Thus the chances are high that plants either accumulate antimicrobials in latent form or produce them from scratch when they become aware of microbial attack, in what is called a phytoalexic response.
A multitude of clinical and in vitro research studies have shown that plant extracts have powerful effects against bacteria, fungi and mycobacteria, even though these products have failed to gain mainstream status due to their being labeled “traditional drugs”. These chemicals are effective in preventing the growth of many reference strains and hospital-acquired strains, and even MRSA or Candida resistant to antifungal agents, in vitro.
They represent a huge pool of molecules which could offer efficacious but inexpensive alternatives to antibiotics. Tohidpour et al performed a comparison of a certain essential oil with many standard antibiotic drugs. Astonishingly, the oil had higher effect on restricting MRS growth in clinical terms compared to these drugs, as well as activity against other standard strains of bacteria.
Chandra et al provided a list of 28 antimicrobial-producing plants which yielded active phytochemicals against resistant bacteria, after reviewing multiple plant-based antimicrobial drugs. It was emphasized that phytochemicals have a distinctive structure at molecular level which is different from that of the antibiotics derived from microbes. This difference is key to developing new antibacterial classes which act in modes that are independent of those exercised by currently used compounds, such as inhibition of protein synthesis. The possibility that phytochemicals may act in new ways or against novel targets is being studied, such as the targeting of type II fatty acid synthase (FAS-II), and this offers enormous promise to phytochemicals as leading candidates to overcome the superbacteria.
In short, phytochemicals could take over the world of antimicrobials by their inexpensive, ubiquitous and powerful characteristics. In place of the dramatic upsurge in the cost of finding a new drug, phytochemical research offers drugs where they can be literally had for the picking. This is especially important for developing nations with limited resources, as their own plants may yield drugs for their own use. Their mechanisms of use, unknown as of now, could herald the arrival of potent and irresistible antimicrobials.
References
- K. C. Nicolaou, Jason S. Chen, David J. Edmonds, and Anthony A. Estrada, Recent Advances in the Chemistry and Biology of Naturally Occurring Antibiotics, Angew. Chem. Int. Ed. 2009, 48, 660 – 719
- Michael A. Fischbach and Christopher T. Walsh, Antibiotics for Emerging Pathogens, Science 325, 1089 (2009).
- The Race Against Drug Resistance A Report of the Center for Global Development’s Drug Resistance Working Group, Rachel Nugent, Emma Back, Alexandra Beith, 2010 by the Center for Global Development.
- Gibbons, Simon. "Phytochemicals for bacterial resistance-strengths, weaknesses and opportunities." Planta medica 74.06 (2008): 594-602.
- Patrick H. Warnke, Stephan T. Becker, Rainer Podschun, Sureshan Sivananthan, Ingo N. Springer, Paul A. J. Russo, Joerg Wiltfang, Helmut Fickenscher, Eugene Sherry, The battle against multi-resistant strains: Renaissance of antimicrobial essential oils as a promising force to fight hospital-acquired infections, Journal of Cranio-Maxillofacial Surgery (2009) 37, 392-397.
- A.Tohidpour, M.Sattari, R.Omidbaigi, A.Yadegar, J.Nazemi, Antibacterial effect of essential oils from two medicinal plants against Methicillin-resistant Staphylococcus aureus (MRSA), Phytomedicine 17 (2010) 142–145.
- Chandra, Harish, et al. "Antimicrobial Resistance and the Alternative Resources with Special Emphasis on Plant-Based Antimicrobials—A Review." Plants 6.2 (2017): 16.

About Metaa Dynamics
Metaa Dynamics is a company where you can find all the stages of scientific discovery, product commercialization and proactive marketing.
Sponsored Content Policy: News-Medical.net publishes articles and related content that may be derived from sources where we have existing commercial relationships, provided such content adds value to the core editorial ethos of News-Medical.Net which is to educate and inform site visitors interested in medical research, science, medical devices and treatments.