A new study uncovers how GIPR signaling in brain cells helps GLP-1 weight-loss drugs bypass the blood-brain barrier and amplify their appetite-suppressing effects, offering a mechanistic explanation for the clinical power of co-agonists.
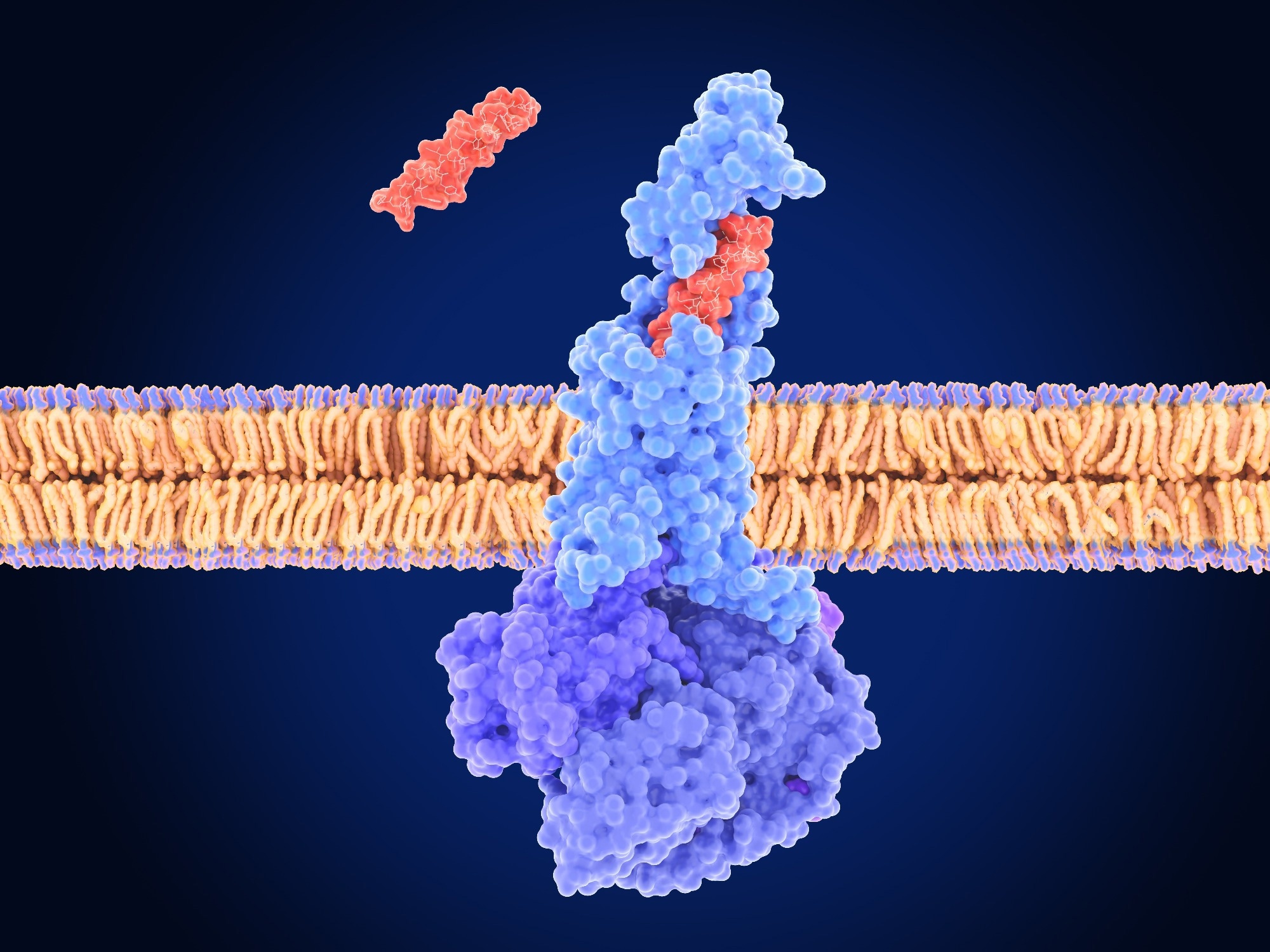 Study: Glucose-dependent insulinotropic polypeptide receptor signaling in oligodendrocytes increases the weight-loss action of GLP-1R agonism. Image Credit: Juan Gaertner / Shutterstock
Study: Glucose-dependent insulinotropic polypeptide receptor signaling in oligodendrocytes increases the weight-loss action of GLP-1R agonism. Image Credit: Juan Gaertner / Shutterstock
In a recent study published in the journal Cell Metabolism, a group of researchers tested whether glucose-dependent insulinotropic polypeptide receptor (GIPR) signaling in oligodendrocytes (OLs) increases brain access and weight-loss efficacy of glucagon-like peptide-1 receptor (GLP-1R) agonists.
Background
One in eight adults lives with obesity, and many now use incretin drugs that can cut weight by over 20%. Incretins act through GIPR and GLP-1R, but why combining them helps remains unclear. The median eminence (ME), an interface where blood signals meet neurons, may be a gate.
OLs, long known for making myelin, also remodel this gate in response to diet. Clarifying whether glucose-dependent insulinotropic polypeptide (GIP) signaling in OLs boosts brain entry and the effects of glucagon-like peptide-1 (GLP-1) therapies could guide stronger treatments; further research is needed.
About the study
The researchers used adult mice to test whether GIPR signaling in OLs shapes brain access and efficacy of GLP-1R agonists. They generated inducible OL knockouts by crossing proteolipid protein 1-Cre recombinase-estrogen receptor T2 (Plp1-CreERT2) with Gipr floxed mice, triggered recombination with tamoxifen at postnatal day 60, and induced obesity with a 60% high-fat diet. A long-acting GIPR agonist (LAGIPRA) and a long-acting GLP-1R agonist (LAGLP-1RA; liraglutide) were administered alone or together.
To map drug entry, a short-acting GLP-1R agonist labeled with IR800 (IR800-Exendin-4) was injected; brains were cleared and imaged by light-sheet microscopy. Oligodendrogenesis and myelination were quantified by fluorescent in situ hybridization and immunostaining for myelin basic protein, breast carcinoma amplified sequence 1, and bone morphogenetic protein 4, with a 5-ethynyl-2′-deoxyuridine pulse-chase.
Vascular permeability was assessed by vascular endothelial growth factor A (VEGF-A) expression, vascular endothelial growth factor (VEGF) immunoreactivity, and mouse endothelial cell antigen 32 (MECA32)-positive fenestrated capillaries. Metabolic readouts included energy expenditure, food intake, and glucose and insulin tolerance.
Finally, an adeno-associated virus encoding the inhibitory human muscarinic M4 receptor engineered for activation by designer drugs (hM4Di) targeted paraventricular hypothalamus (PVH) arginine vasopressin (AVP) neurons in arginine vasopressin promoter-Cre (Avp-Cre) mice; deschloroclozapine was administered to activate hM4Di and suppress these neurons during liraglutide tests.
Study results
In the ME, GIPR was enriched in mature OLs, with rare expression in OL progenitor cells; high-fat feeding increased OL density and the number of GIPR-positive OLs specifically in this region. This effect was not observed in white matter tracts such as the corpus callosum, indicating a localized role.
OL-specific GIPR deletion reduced adult oligodendrogenesis and OL survival in the ME and lowered myelin basic protein, while major white-matter tracts showed little change, indicating a localized role at the brain’s metabolic gateway. Mice lacking OL GIPR showed reduced energy expenditure and intake, preserved oral glucose tolerance, impaired insulin tolerance, and shifts in branched-chain–related metabolites, consistent with altered substrate handling during obesity.
Pharmacologic activation produced complementary effects. In lean mice, a long-acting GIPR agonist increased OL lineage cells and myelin in the ME. In diet-induced obesity (DIO), the same agonist increased new OL production and restored turnover, while raising vascular access signals: VEGF-A transcripts and VEGF immunoreactivity increased, and MECA32-marked fenestrated capillaries became denser, indicating enhanced vascular permeability.
Pre-treating obese mice with the GIPR agonist increased the brain uptake of an IR800-labeled short-acting GLP-1R agonist in the ME and adjacent arcuate nucleus of the hypothalamus (ARH), indicating enhanced access across the ME-ARH border. Crucially, this uptake increase required OL GIPR; it was absent after OL GIPR deletion.
Efficacy mirrored entry, as in wild-type mice, long-acting GLP-1R agonism lowered food intake and body weight, and co-administration with the GIPR agonist amplified both outcomes; in OL GIPR knockouts, the GIPR agonist no longer potentiated GLP-1R-driven weight loss or anorexia, indicating that OL GIPR signaling is required for full synergy.
Imaging showed that peripherally dosed short-acting GLP-1R agonists accumulated along myelinated axon bundles in the ME, colocalizing with myelin basic protein; revealing a novel mechanism: peripherally administered GLP-1R agonists access the brain via myelinated AVP axons in the ME, bypassing the blood-brain barrier (BBB).
Super-resolution microscopy localized GLP-1R on AVP axons and at nodes labeled by contactin-associated protein (CASPR). Finally, chemogenetic silencing of PVH AVP neurons with deschloroclozapine prevented liraglutide-induced hypophagia and weight loss, demonstrating that these neurons are necessary for the systemic drug’s weight-loss action.
Conclusions
To summarize, this study connects incretin pharmacology to a concrete brain entry mechanism: signaling through GIPRs in ME OLs increases vascular permeability via VEGF-A induction and increased capillary fenestration and enables GLP-1R agonists to reach appetite-regulating AVP axons.
The requirement for this pathway may help explain why GIPR/GLP-1R co-agonists show greater efficacy than single agents, and offer a mechanistic basis for their enhanced clinical performance. Clinically, the mechanism helps interpret the potency of co-agonists used for obesity and type 2 diabetes and points to biomarkers, such as VEGF-A induction or imaging of ME access, to guide dosing or combinations while limiting side effects.
However, the authors note several limitations: the OL Gipr knockout model achieved only partial deletion; the experiments primarily assessed liraglutide rather than other GLP-1R agonists; and the behavioural outcomes, while informative, were not exhaustive. These caveats temper the conclusions and highlight the need for further research to confirm generalizability and clinical relevance.
Journal reference:
- Hansford, R., Buller, S., Tsang, A. H., Benoit, S., Roberts, A. G., Erskine, E., Brown, T., Pirro, V., Reimann, F., Harada, N., Inagaki, N., Samms, R. J., Broichhagen, J., Hodson, D. J., Adriaenssens, A., Park, S., & Blouet, C. (2025). Glucose-dependent insulinotropic polypeptide receptor signaling in oligodendrocytes increases the weight-loss action of GLP-1R agonism. Cell Metabolism. DOI: 10.1016/j.cmet.2025.07.009, https://www.cell.com/cell-metabolism/fulltext/S1550-4131(25)00355-9