Most people with asthma need two kinds of medicines: quick-relief medicines, to be taken when you need them, for immediate relief of your symptoms, and long-term control medicines, to be taken daily, for a long time, to stop and control the inflammation in your airways and thereby prevent symptoms and attacks.
Everyone with asthma needs a quick-relief or rescue medicine to stop asthma symptoms before they get worse. An inhaled short-acting beta2-agonist is the preferred quick-relief medicine. It acts quickly to relax tightened muscles around your airways so that your airways can open up and allow more air to flow through.
You should take your quick-relief medicine at the first sign of any asthma symptoms. Your doctor may recommend that you take this medicine at other times, for example, before exercise.
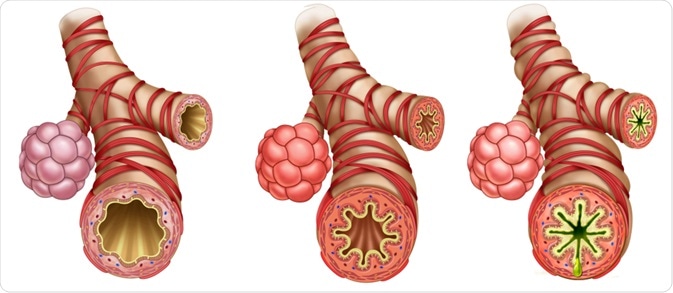 This illustration shows a healthy bronchus, an inflamed bronchus, and a bronchus suffering from severe asthma. Image Credit: ilusmedical / Shutterstock.com
This illustration shows a healthy bronchus, an inflamed bronchus, and a bronchus suffering from severe asthma. Image Credit: ilusmedical / Shutterstock.com
When to take long-term medicines
Quick-relief medicines are very good at stopping asthma symptoms, but they do nothing to control the inflammation in your airways that produces these symptoms. If you need to use more quick-relief medicine than usual or if you need to use it every day, it may be a sign that you also need to take a long-term control medicine to reduce the inflammation in your airways. Discuss this with your doctor as soon as possible.
Long-term control medicines are used to prevent asthma symptoms from coming on in the first place. These medicines work more slowly than quick-relief medicines, and you may need to take them for several weeks before you feel their effects. Once your asthma is under control, you may be able to cut back on some of these medicines.
The most effective long-term control medicines are anti-inflammatory medicines. They reduce the inflammation in your airways, making the airways less irritable and less likely to react to your asthma triggers.
Anti-inflammatory medicines are usually most effective when you take them every day, even when you don't have any symptoms.
The most effective anti-inflammatory medicines for most people are inhaled corticosteroids.
Some people do not like the idea of taking steroids. But the inhaled corticosteroids used to treat asthma have been studied over the years in large groups of adults and children as young as 2 years old and have been found to be generally safe when taken as directed by your doctor.
They also are very different from the illegal anabolic steroids taken by some athletes. They are not habit-forming-even if you take them every day for many years. And, because they are inhaled, the medicine goes right to your lungs where it is needed.
Like many other medicines, inhaled corticosteroids can have side effects. But most doctors agree that the benefits of taking them and preventing attacks far outweigh the risks of side effects.
Common advice is to take inhaled corticosteroids as your doctor prescribes and use a spacer or holding chamber with your inhaler to make sure the medicine goes directly to your lungs. It is also a good idea to rinse your mouth out with water after taking these medicines.
Other long-term control medicines available to treat asthma include:
- Inhaled long-acting beta2-agonists. These are bronchodilators that can help prevent symptoms when taken with inhaled corticosteroids. These medicines should not be used alone. They also should not be used to treat serious symptoms or an attack.
A two-in-one medicine containing corticosteroids and long-acting beta2-agonists is now available.
- Cromolyn sodium is a nonsteroidal anti-inflammatory medicine that can be used to treat mild persistent asthma, especially in children. It is not as effective as inhaled corticosteroids.
- Leukotriene modifiers, or anti-leukotriene medicines, are a newer class of long-term control medicines that block the action of chemicals in your airways. If not blocked, certain chemicals, called leukotrienes, increase the inflammation in your lungs during an asthma attack.
Anti-leukotriene medicines, which are available in pill form, are used alone to treat persistent asthma or with inhaled corticosteroids to treat moderate asthma. They are not as effective as inhaled corticosteroids for most patients.
- Theophylline, also available in pill form, acts as a bronchodilator to relax and open the airways. It can help prevent nighttime symptoms. It is sometimes used alone to treat mild persistent asthma, but most of the time it is used with inhaled steroids.
If you take theophylline, you need to have your blood levels checked regularly to make sure the dose is right for you.
Taking your medicines
Inhalers
Many asthma medicines, both quick-relief and long-term control types, come as sprays and powders in an inhaler. An inhaler is a hand-held device that delivers the medication right to the airways in your lungs where it is needed. There are several kinds of inhalers.
The metered-dose inhaler (MDI) is a small canister that delivers a measured dose of medicine through your mouth to your airways. Some MDIs use a chemical to push the medicine out of the inhaler. Inhalers that use the chemical chlorofluorocarbon (CFC) are gradually being replaced.
Other types of inhalers include:
- A breath-activated inhaler from which you simply breathe in by mouth and the medicine comes out in a soft spray
- A dry powder inhaler (DPI)
- A Turbuhaler
- An Aerolizer
It is important for you to learn how to use your inhaler correctly. Read the instructions that come with it and ask your health care provider or pharmacist to show you how to use it. Then try it yourself and ask him or her to make sure you are using it the right way.
.jpg) Asthma medication is often taken via an inhaler. Image Credit: New Africa / Shutterstock.com
Asthma medication is often taken via an inhaler. Image Credit: New Africa / Shutterstock.com
Spacers
A spacer or holding chamber can make using an MDI a lot easier. It is an especially good idea to use a spacer with corticosteroid MDIs as it decreases the amount of medicine that lands on your tongue or in the back of your mouth. This reduces irritation to your throat and increases the amount of medicine that gets down into your lungs where it belongs.
There are many kinds of spacers. Some have a mouth piece. Some have a face mask that comes in different sizes to fit both children and adults.
Many spacers fit on the end of an inhaler; for some, the canister of medication fits into the device. Some MDIs come with builtin spacers.
Spacers are not needed for dry powder devices.
Most spacers also come with instructions on how to use them. It is important to ask your health care provider to show you how to use a spacer with your MDI. Then try it yourself and ask them to make sure you are doing it correctly.
Nebulizers
A nebulizer is another device that makes it easier to take inhaled medicines. It provides the medicine in a fine mist, rather than a spray. Using a nebulizer is usually easy; you simply breathe in and out normally through a mask or mouthpiece connected to the nebulizer. But it takes more time to use than an inhaler. It also is more expensive and requires more maintenance. Instructions for using different nebulizers vary, so follow the instructions on the package insert.
Nebulized asthma medication may be especially useful for infants, young children, and adults who have trouble using an inhaler.
Regardless of which of these devices you use, you have to use them the right way, or you will not get all the medicine into your lungs.
The best way to learn to use these devices correctly is to ask your doctor or a nurse, pharmacist, or respiratory therapist to show you how. Then demonstrate it back to them to make sure you have it right.
What medicines do I need?
Doctors usually decide which medicines and how much of each to prescribe based on your lung function and your pattern of symptoms - how many days and nights you have them, as shown on the chart below. Usually, if you have symptoms no more than 2 days a week or 2 nights a month, they will consider your asthma to be mild and intermittent and prescribe only quick-relief medicines to be used when you have symptoms.
If you have more frequent symptoms, you probably need daily long-term control medicines to prevent symptoms. It may take several visits before the doctor finds exactly the right medicines and doses for you.
| |
Days With Symptoms |
Nights With Symptoms |
| Intermittent asthma |
No more than 2 days each week |
No more than 2 nights each month |
| Mild persistent asthma |
3 days or more a week but no more than one bout of symptoms on any 1 day |
3 nights or more a month |
| Moderate persistent asthma |
Every day |
More than 1 night a week |
| Severe persistent asthma |
Throughout the day every day |
Often |
Now that you know more about asthma medicines and what they do, ask your doctor to write on your asthma action plan:
- The name of each of your quick-relief and long-term control medicines
- How much of each medicine you should take
- When to take each of your medicines
Other measures for treating asthma include:
- Allergy shots (immunotherapy) may help if you have allergies that cannot be easily controlled by avoiding your triggers and taking medicine.
- Older people with asthma should have pneumococcal (pneumonia) vaccinations.
- Antibiotics are not recommended for either routine or emergency treatment of asthma, except, as needed, for a bacterial infection, such as pneumonia or suspected bacterial sinusitis.
Your asthma triggers and how to avoid them
Avoiding the things that bring on your asthma symptoms (your asthma triggers) is another important part of your asthma action plan.
Some of the most common things that bring on asthma symptoms are allergens, irritants, viral infections, and exercise.
Allergens are substances that can cause you to have an allergic reaction. That is, in some people, the immune system sees them as "foreign" or "dangerous" and reacts in an exaggerated way to protect the body against them.
Asthma triggers
Some of the most common allergens for people with asthma are:
- Animal dander - scales or dried saliva from the hair, skin, or feathers of animals
- Dust mites - tiny bugs that thrive in mattresses, upholstered furniture, carpets, and stuffed animals
- Cockroach droppings
- Pollen from trees and grass
- Molds, both indoor and outdoor
Irritants are things in the environment that may irritate your lungs. Some of the most common lung irritants are:
- Cigarette smoke
- Air pollution, including ozone
- Cold air or changes in weather like freezing temperatures, high humidity, and thunderstorms
- Strong odors or sprays, such as perfumes, household cleaners, cooking fumes - especially from frying, paints, or varnishes
Other things that bring on asthma symptoms in some people include:
- Exercise
- Respiratory infections, such as colds or viral pneumonia, sinusitis and rhinitis.
- Medicines, such as aspirin or other nonsteroidal anti-inflammatory drugs (NSAIDS) like ibuprofen, and beta-blockers, which are used in high blood pressure and glaucoma medicines
- Sulfites in food (dried fruit, processed potatoes, or shrimp) or beverages (wine or beer)
- Gastroesophageal reflux disease (GERD), a medical condition that causes heartburn
- Strong expressions of emotion (including laughing hard or crying)
This is not a complete list of all the things that can bring on your asthma symptoms. It is important for you to learn what causes problems for you.
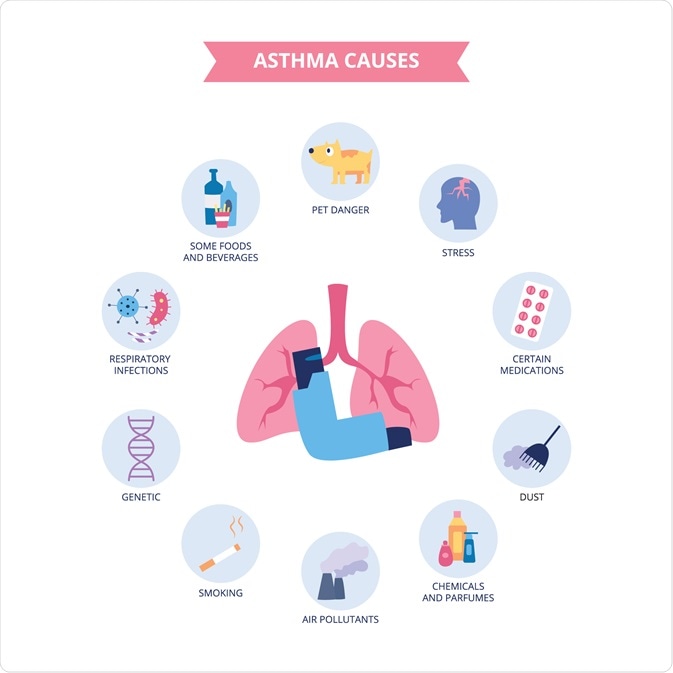 Infographic of asthma causes. Image Credit: Antonov Maxim / Shutterstock.com
Infographic of asthma causes. Image Credit: Antonov Maxim / Shutterstock.com
How to remember to take your medicines
- Keep your medicine on the night stand next to your side of the bed.
- Take your asthma medicine right after you brush your teeth and keep it with your toothbrush as a reminder, or put it next to your cereal box and take it with breakfast.
- Put "sticky" notes in visible places to remind yourself to take your asthma medicine, e.g. on the refrigerator.
- If you use the telephone company's voice mail service, record a reminder for yourself, and the service can automatically call you every day at the same time.
- Establish a buddy system with a friend who also is on daily medication and arrange to call each other every day with a reminder to "take your medicine."
- Place your medicine in a weekly pill box, available at most pharmacies.
- If you have a personal computer, program a start-up reminder to take your asthma medicine or sign up with one of the free services that will send you reminder e-mail every day.
- If you have a watch with an alarm, program it to beep and remind you to take your asthma medicine.
- Remember to refill your prescription. Each time you pick up a refill, make a note on your calendar to order and pick up the next refill one week before the medicine is due to run out.
Pharmacology - DRUGS FOR ASTHMA AND COPD (MADE EASY)
Further Reading
Last Updated: Jan 29, 2021