Radioembolization is a generally painless procedure for liver cancer that directly targets the blood supply to the tumor site. Approximately 70% to 95% of patients will experience improvements in liver-related symptoms, with survival rates improving from months to years following this procedure. Taken together, radioembolization is a palliative treatment, meaning it relieves symptoms but does not provide a cure.
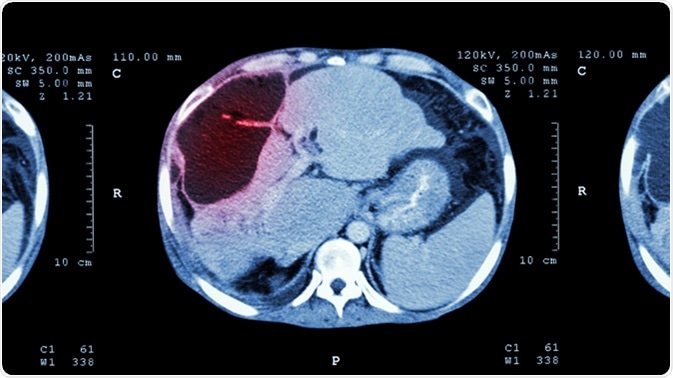
Image Credit: Puwadol Jaturawutthichai / Shutterstock
What is liver cancer?
Liver cancer is a serious type of cancer that starts in the liver and is sometimes called hepatic cancer. The most common type of liver cancer is hepatocellular carcinoma (HCC), which is the sixth most common malignancy worldwide. Symptoms of HCC include weight loss, jaundice, itching, nausea, swollen abdomen, loss of appetite, and a lump in the right side of the abdomen.
What is radioembolization?
Radioembolization is a treatment for liver cancer that combines radiation therapy and embolization. This procedure involves the insertion of tiny glass beads called microspheres into blood vessels that feed the tumor in order to block the blood supply to the cancer cells. The beads, which are smaller than a human hair in width, are filled with the radioactive isotope yttrium Y-90.
Radioembolization is a minimally invasive procedure. While it is not a cure for liver cancer, it alleviates symptoms and slows the progression of the cancer.
How does radioemobilization work?
Radioemobilization uses contrast agents which are used to improve the visibility of the blood vessels, as well as X-ray imaging. A catheter, which is a thin plastic tube, is inserted into the femoral artery and moved into the treatment area. The microspheres are also inserted through a catheter and advanced to the blood vessels that supply the tumour with blood. The high dose of radiation to the cancer cells starves the cells of the oxygen and nutrients necessary for growth.
The microspheres remain inside the liver after the yttrium-90 radiation has disappeared over a period of 30 days. Despite residing in the liver for this amount of time, the radioactive isotope typically will not cause any harm to the individual. The microspheres only give off radiation over an area of a few square millimeters, thereby reducing the potential damage to surrounding tissues.
The procedure
Overall, radioembolization is painless and takes around an hour to complete. An anesthetic is used to numb the intravenous incision site in the groin and sedatives are sometimes used to relax the patient during the procedure.
Brief pain may be experienced while the microspheres are injected along with a short-term feeling of warmth as the contrast agents pass through the body. Some patients also feel the need to pass urine.
It is important that the patient limits their contact with other people after the radioembolization. Additional suggestions for at least seven days after the procedure advise against:
- Sharing a bed with other people.
- Sitting next to people on public transport for more than two hours.
- Making close contact with children or pregnant women.
Side effects of radioembolization are mild, and commonly include:
- Raised temperature
- Chills
- Nausea
- Diarrhea
- Stomach pain
- Fatigue lasting up to six weeks
- Pressure in the abdomen
Rare side effects include:
- Gut irritation, which can be prevented by anti-ulcer medication for four weeks after treatment.
- Lung damage. In the event that the patient experiences cough and/or shortness of breath, treatment with steroids may be initiated.
- Liver inflammation might present a few weeks after treatment and require regular monitoring.
- Gallbladder inflammation (cholecystitis)
Benefits
- As well as improving the quality of life, radioembolization can extend the life of a patient with inoperable tumors from months to years
- Compared with standard radiation therapy, radioembolization presents fewer side effects and delivers a higher dose of radiation than external beam therapy
- No surgical incision is required to perform the procedure and any incisions made do not require sutures
Risks
- Small risk of infection from skin penetration.
- Small risk of allergic reactions to contrast agents
- Infection, bleeding, or bruising at the catheter puncture site
- Damage to blood vessels rarely occurs
- Ulcers in the stomach or duodenum if the microspheres settle in the wrong place
- Infection after the procedure, even after antibiotics are given
Several measures have been put in place to limit and control the risks of radioembolization.
After the procedure, some patients experience side effects called post-emobilization syndrome. The symptoms of this syndro,e include fatigue, fever, nausea, and vomiting.
Patients may also experience pain after the procedure due to the ischemia of the treated area. Oral or intravenous medications are typically sufficient to control this side effect. Typically, most side effects will pass within five days.
Conclusion
Radioembolization is a minimally invasive treatment that provides relief from symptoms but does not provide a cure for liver cancer. As with any treatment, there are risks and side effects; however, extensive measures are put in place before the procedure is done to limit the incidence of complications. Overall, radioembolization presents fewer side effects than external beam therapy, and targets the blood supply to the tumor directly.
References
Further Reading
Last Updated: Apr 20, 2021