The condition known as von Willebrand disease is caused by a deficiency in the quantity or quality of von Willebrand factor (vWF), a key component of the coagulation cascade.
Diagnosis starts with eliciting a personal or family history of abnormal bleeding along with diagnostic test results. This should be the basis of suggesting further tests since the practical usefulness of diagnosing vWF may be low in dubious cases.
History may be considered suggestive of abnormal bleeding if there are:
- 3 or more symptoms of bleeding
- A bleeding score (using any standard questionnaire) of 3 (males) or 5 (females). This is generated by summing the severity of all the bleeding symptoms reported by an individual, followed by grading them on a predetermined scale. The questionnaire developed by the International Society for Hemostasis and Thrombosis is one frequently used in this assessment.
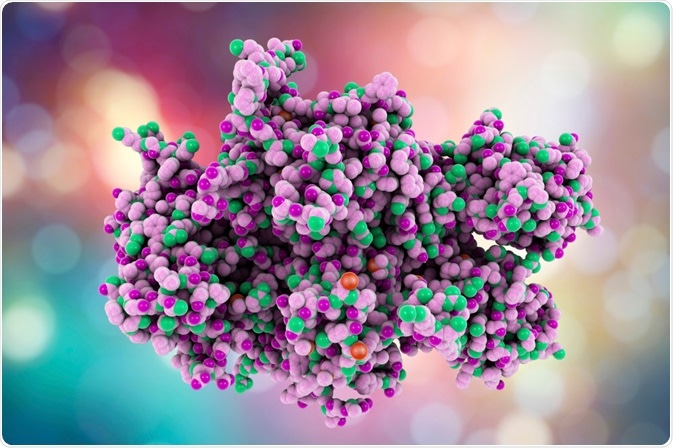 Coagulation factor VIII. Image Credit: Kateryna Kon / Shutterstock.com
Coagulation factor VIII. Image Credit: Kateryna Kon / Shutterstock.com
Primary tests
These tests include:
- A total blood count, which includes:
- hemoglobin (normal or low depending upon the severity of blood loss)
- hematocrit (normal or low depending upon the severity of blood loss)
- platelet count and morphology (usually normal, count low in type 2 vWD)
- prothrombin time (usually normal)
- activated partial thromboplastin time (normal or prolonged, the latter if FVIII levels are reduced)
- fibrinogen (optional, usually normal)
- thrombin time (optional, usually normal)
- vWD profile:
- vWF:RCo, a functional assay that tests for the ability of vWF to adhere to normal platelets in the presence of the antibiotic ristocetin, which acts as a cofactor
- vWF:Ag which assays the amount of reduced vWF antigen in plasma using enzyme-linked immunosorbent assay (ELISA) or latex immunoassay (LIA)
- FVIII:C which tests the coagulant activity of factor VIII, which depends on the normal carrier activity of vWF
- ABO blood grouping – in type O individuals, levels of both vWF:Ag and vWF:RCo are normally much lower than average when compared with other blood types, making it more difficult to diagnose vWF in this blood group
Specialized coagulation tests
Once the diagnosis is confirmed, additional tests may be done, such as:
- vWF multimer analysis for assigning the type and subtype of the disease, depending on the size and distribution of multimers. SDS-agarose electrophoresis is used to differentiate low, intermediate and high molecular weight multimers and oligomers of vWF subunits. High molecular weight multimers are reduced or absent in types 2A and 2B.
- vWF:CBA, which assays the collagen-binding activity of vWF. This in turn, depends on larger multimers that bind collagen more avidly and help differentiate the subtypes. A defect in collagen binding may also cause it.
- vWF:FVIIIB, which is a test to measure the ability of vWF to bind to factor VIII, preventing its rapid catabolism and maintaining normal FVIII levels. This is low or absent in type 2N.
- RIPA, or ristocetin-induced platelet aggregation, occurs only in type 2 or platelet-type (or pseudo-) vWD at low ristocetin concentrations.
Factor VIII levels are usually higher than vWF levels in type 1 vWD and may be normal. FVIII is 2-3 times higher than vWF in type 2, except in type 2N, in type 3, it is very low, less than 10 IU/dL.
Molecular diagnosis
The molecular diagnosis of vWD does not usually require the characterization of the exact mutation. The gene which codes for this protein is on chromosome 12p13.2, and is a large 178 kb gene with 52 exons. Mutations in exon 28 have been identified in type 2A and 2B. These mutations code for the reactive region of the vWF subunit that binds to platelet glycoprotein Ib (GPIb). Mutation analysis helps to differentiate various subtypes of type 2 vWD.
However, identifying the mutation that causes type 2N disease is important because it enables us to rule out the carrier state for hemophilia A, and is thus useful in genetic counseling. Type 2N is inherited in an autosomal recessive manner and vWF mutations are present, unlike normal vWF genes and an X-linked inheritance in hemophilia A.
In type 2B again, identification of the exact defect is important to distinguish it from a similar-appearing platelet-defect-induced vWD due to mutations in the GP1BA gene.
References
Further Reading
Last Updated: Jan 31, 2021