Any substance that induces the immune system to produce antibodies against it is called an antigen. Any foreign invaders, such as pathogens (bacteria and viruses), chemicals, toxins, and pollens, can be antigens. Under pathological conditions, normal cellular proteins can become self-antigens.
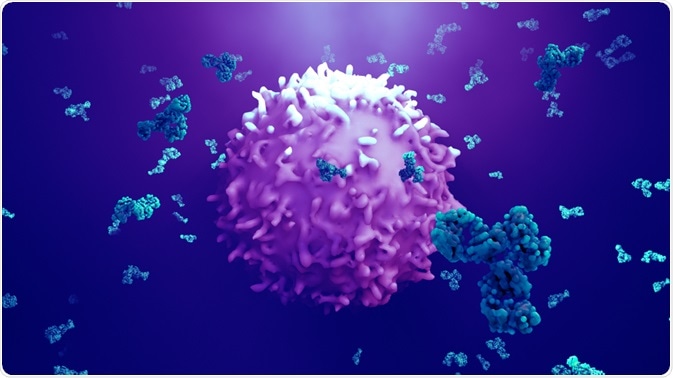
Image Credit: Design_Cells/Shutterstock.com
What is an antigen?
In general, antigens are composed of proteins, peptides, and polysaccharides. Any portion of bacteria or viruses, such as surface protein, coat, capsule, toxins, and cell wall, can serve as antigens.
Moreover, a combination of lipid or nucleic acid with proteins or polysaccharides can form more complex antigens, such as lipopolysaccharides. Lipopolysaccharides are significant ingredients of endotoxins produced by gram-negative bacteria.
An antigen contains distinct sites on its surface, called an epitope or antigenic determinant. Antibodies generated against an antigen recognize and interact with specific epitopes via antigen-binding sites (paratopes) to trigger immune responses.
What are the types of antigens?
Antigens are mainly categorized based on their origins. For example, antigens that enter the body from outside via ingestion, inhalation, or injection are termed exogenous antigens. These include pathogens, chemicals, toxins, allergens, pollens, etc.
Autoantigens or self-antigens are normal cellular proteins or a complex of proteins that are mistakenly attacked by the immune system, leading to autoimmune diseases. A normal self-protein becomes a self-antigen because of impaired immunological tolerance, caused by genetic or environmental factors.
Tumor antigens are produced due to tumor-specific mutations that occur during the neoplastic transformation of normal cells into cancerous cells. These antigens are expressed on the cancer cell surface to be recognized by the immune system. However, despite expressing cell surface antigens, most cancer cells gain the ability to escape immune system-mediated elimination.
What are haptens?
Haptens are small molecules that can trigger an immune response only when combined with a carrier protein. The hapten–carrier protein complex is called an adduct. Urushiol, an allergen of poison ivy, is an example of hapten that causes contact dermatitis.
After entering the body through the skin, urushiol undergoes oxidation to produce quinone, a reactive molecule. Subsequently, quinone binds to skin protein to form hapten adducts that trigger immune responses.
How do antigens trigger an immune response?
The specificity of the immune response depends on the epitope–paratope interaction. An epitope can be of two types: conformational (discontinuous amino acid sequence of the antigen) and linear epitopes (continuous amino acid sequence of the antigen).
Upon entering the body, an antigen triggers the adaptive immune system that comprises specialized immune cells, such as B and T lymphocytes (B cells and T cells). There are two types of adaptive immune responses: antibody-mediated and cell-mediated immune responses. The antibody-mediated immunity is triggered when antibodies expressed on the B cell surface recognize specific epitopes of an antigen and subsequently internalize the antigen.
The antigen is then presented on the B cell surface to be recognized by helper T cells, which subsequently activate the B cell. Activated B cells rapidly divide to produce two types of cells: 1) plasma cells that produce antigen-specific antibodies, and 2) memory B cells that store antigen-specific information for future protection.
In the cell-mediated immune system, antigen-presenting cells, such as dendritic cells, macrophages, and B cells, internalize and digest the antigen and subsequently present the antigenic fragments on their cell surface through major histocompatibility complex (MHC).
There are two types of MHC molecules: class I MHC molecules (present antigens to cytotoxic T cells) and class II MHC molecules (present antigens to helper T cells). Antigenic fragments associated with MHC are presented to T cells by two different pathways.
In the endogenous pathway, MHC class I molecules present endogenous antigens derived from pathogen-specific proteins produced within infected cells. However, in the exogenous pathway, MHC class II molecules present antigenic fragments derived from pathogens extracellularly.
Upon recognizing the MHC-antigen complex, T cells start secreting cytokines, which in turn facilitate the maturation of T cells. T cells that mature into helper T cells produce more cytokines to further attract and activate macrophages, lymphocytes, and neutrophils. T cells that mature in cytotoxic T cells attack and destroy pathogen-infected cells.
Antigens in medical science
Pathogen-specific antigens can be used as diagnostic markers to detect the current infection status of an individual. Rapid antigen tests are immunoassays used to detect the presence of pathogen-specific proteins in biological samples.
Also, pathogen-specific antigens are used in vaccine production. During vaccine production, pathogen-specific antigens are processed so that they can induce desired immune responses without causing disease.
In tumor vaccines, tumor-specific antigens are used to trigger immune cells that specifically target and destroy cancer cells.
Further Reading
Last Updated: Apr 22, 2022