A tumor is an abnormal growth of cells within the body, usually facilitated by a lack of apoptosis (natural cell death), therefore allowing for uncontrolled growth of unwanted or damaged cells. Tumors can be benign (non-cancerous, usually harmless) or malignant (cancerous, harmful, and can spread further).
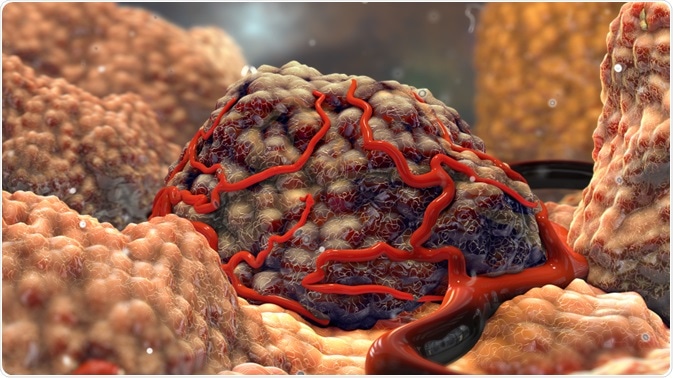
Image Credit: Nathan Davey/Shutterstock.com
What does tumorigenesis mean?
The phrase ‘tumorigenesis’ refers to the initial formation of a tumor in the body. Over the last 50 years, the multiplicity of cancer has been demonstrated to be increasingly palpable via a variety of scientific studies that have previously demonstrated some common characteristics of tumorigenesis as a process.
Of late, a selection of models representing multistep tumorigenesis, such as through small genetic modifications, have been theorized to clarify how the metamorphosis of a normal cell into a potentially dangerous cancer cell could come to be.
How does tumorigenesis occur?
Tissue regeneration and development in mammals takes place via proteins called regulatory growth factors. These factors, therefore, affect many of the parameters surrounding cell development: proliferation, survival, and certain aspects of cell behavior, as well as cell differentiation, are all determined by the delicate balance between inhibitory and stimulatory signals given by these factors.
The exact effect of any of these growth factors is wholly influenced by the concentration of said factor, the type of responding cell, and the existence of external stimuli. For example, some growth factors could accomplish a selection of functions when put under alternative circumstances.
Human tumorigenesis can be considered to be the accumulation of genetic mutations within cells that affect both the tumor suppressor genes as well as the oncogenes. However, it has been determined through scientific studies that common adult cancers do not tend to have the commonly understood mutations previously outlined as critical during some of the earlier stages of tumorigenesis.
APC Gene
In a study from the early 1990s, it was determined whether or not mutations of a certain ‘APC’ gene could play such a role in a common adult cancer: human colorectal tumors, which had already been proven to evolve from smaller, benign tumors (otherwise known as adenomas) into large, malignant tumors called carcinomas. This process occurs over an extended period (10+ years).
It was reported in this study that the genetic sequence analysis of 41 different colorectal tumors exposed that the greater part of colorectal carcinomas (60% of them) and adenomas (63% of them) were found to have contained some form of mutated APC gene.
Additionally, this APC gene was discovered to have met two of the criteria of importance for tumorigenesis. Firstly, any mutations of this certain gene were observed inside the smallest, earliest-presenting tumors that could be successfully analyzed, which included some adenomas as little as 50 mm in diameter.
Secondly, the recurrence of these mutations was found to remain consistent as the tumors advanced from the early benign stages, all the way to the much later malignant stages.
AP-1 Transcription Factor
There have been many other more recent studies exploring how tumorigenesis works, such as observing the significance of AP-1 transcription factor composition during the process of tumorigenesis.
This influence was put to the test by using AP-1 monomers joined by flexible polypeptides to force a specific protein pairing. This approach using single-chains demonstrated that, for example, c-Jun and Fra2 proteins inhibited the growth arrest of the immortalized fibroblasts at assemblage (whilst also under low-serum conditions), but the pairings of c-Jun–Fra1 or c-Jun–c-Fos did not.
Additionally, the oncogenic potential of specific AP-1 dimers has also been recently studied by making use of dimer-specific mutations of these AP-1 proteins with these experiments proving that the c-Jun-induced program of transformation can easily be separated into separate pathways: using c-Jun–Atf activity triggered both c-Jun–c-Fos activity and growth-factor independence, causing anchorage-independent growth and tumorigenesis.
This, therefore, showed the process of cellular invasive growth and angiogenesis, also indicating a differential requirement for N-terminal c-JUN phosphorylation in tumorigenesis
The first of many anti-angiogenesis clinical trials tested on human cancer patients have not presented results akin to the initial high expectations: they did not significantly reduce tumor burden, which would have therefore prolonged life, as was seen in many of the pre-clinical studies performed in the 1990s.
Tumorigenesis is becoming better understood by molecular biologists, which could soon indicate possible cancer prevention methods as demonstrated by these previous studies.
Sources
Baardwijk A.V. et al. (2006). The current status of FDG–PET in tumor volume definition in radiotherapy treatment planning. https://doi.org/10.1016/j.ctrv.2006.02.002
Bergers, G. & Benjamin, L. E. (2003). Tumorigenesis and the angiogenic switch. http://dx.doi.org/10.1038/nrc1093
Powell, S. M et al. (1992). APC mutations occur early during colorectal tumorigenesis. https://search.proquest.com/docview/204435379?accountid=14685
Eferl R. and Wagner E.F. (2003). AP-1: A Double-Edged Sword in Tumorigenesis. DOI:10.1038/nrc1209
Further Reading
Last Updated: Jan 30, 2020