Introduction
Preventing RSV
What is nirsevimab?
Supporting clinical data
Policy and access
Conclusions
References
Further reading
Emerging clinical evidence shows that nirsevimab can extend powerful, single-dose RSV protection to all infants, reshaping how we safeguard babies during their most vulnerable months.
 Image Credit: comzeal / Shutterstock.com
Image Credit: comzeal / Shutterstock.com
Introduction
Respiratory syncytial virus (RSV) is the leading cause of hospitalization in infants, with recent global estimates indicating that RSV causes tens of millions of lower respiratory tract infections and several million hospitalizations in children under five years of age each year. Preventing RSV infection in young children, particularly infants who are particularly vulnerable to serious complications, remains challenging, as palivizumab is only indicated for high-risk infants while also requiring monthly dosing.1,5
There remains an urgent need for long-lasting passive protection that can be administered to all infants, ideally as a single dose covering an entire season, to reduce hospitalizations and downstream respiratory morbidity.1 This article explains how nirsevimab, a long-acting monoclonal antibody, can provide season-long RSV protection for infants while summarizing trials, safety, policy, and access.
Preventing RSV
Palivizumab and maternal vaccination represent two established approaches to protecting infants against RSV. Palivizumab is a monoclonal antibody directed at the RSV fusion protein and has been used for over 20 years in high-risk infants.1,2
Importantly, palivizumab use requires monthly dosing throughout the RSV season to maintain protective levels. Although this limits feasibility for universal programs, palivizumab remains valuable for infants with prematurity, chronic lung disease, or congenital heart disease who are at the greatest risk of severe disease.2
Maternal RSV vaccination provides passive protection to newborns by increasing maternal antibody levels that are subsequently transferred across the placenta late in pregnancy. In 2023, the United States Food and Drug Administration (FDA) approved Pfizer’s bivalent prefusion F protein vaccine (Abrysvo) for maternal administration between 32 and 36 weeks’ gestation, whereas the European Medicines Agency recommends maternal vaccination between 24 and 36 weeks.
This strategy aims to provide optimal protection during the early months of life when infant vulnerability is highest; however, protection naturally wanes as maternal antibodies decline. Phase III clinical data, including the MATISSE trial, report notable efficacy against medically attended RSV-lower respiratory tract infection (LRTI) in the first 90-180 days of life (around 82% at 90 days and 69% at 180 days, with ~57% efficacy against severe RSV-LRTI), with a generally acceptable safety profile in mothers and infants.2
Whereas palivizumab offers targeted, ongoing protection for high-risk infants, maternal vaccination can provide broad protection at birth for many infants. Thus, programs may combine approaches tailored to local epidemiology, antenatal coverage, and resource constraints to maximize prevention in the first months of life.2
What is nirsevimab?
Nirsevimab is a recombinant human immunoglobulin G1 kappa (IgG1κ) monoclonal antibody designed to prevent RSV infection by binding to a highly conserved site on the RSV fusion (F) protein. Thereafter, the F protein remains in its prefusion state, preventing membrane fusion and viral entry into host cells.3,5
In infants, the mean serum half-life of nirsevimab is about 69 days. Clinical trial pharmacokinetic data and real-world analyses suggest that protection against RSV persists for about five months after a single intramuscular dose of 50 mg for infants weighing under 5 kg and 100 mg for those weighing 5 kg or more.3,5
In a large randomized trial in healthy late-preterm and term infants given one dose before the RSV season, nirsevimab reduced medically attended RSV lower respiratory tract infection while maintaining an overall safety profile similar to placebo, with low rates of antidrug antibodies and no reports of serious hypersensitivity.3
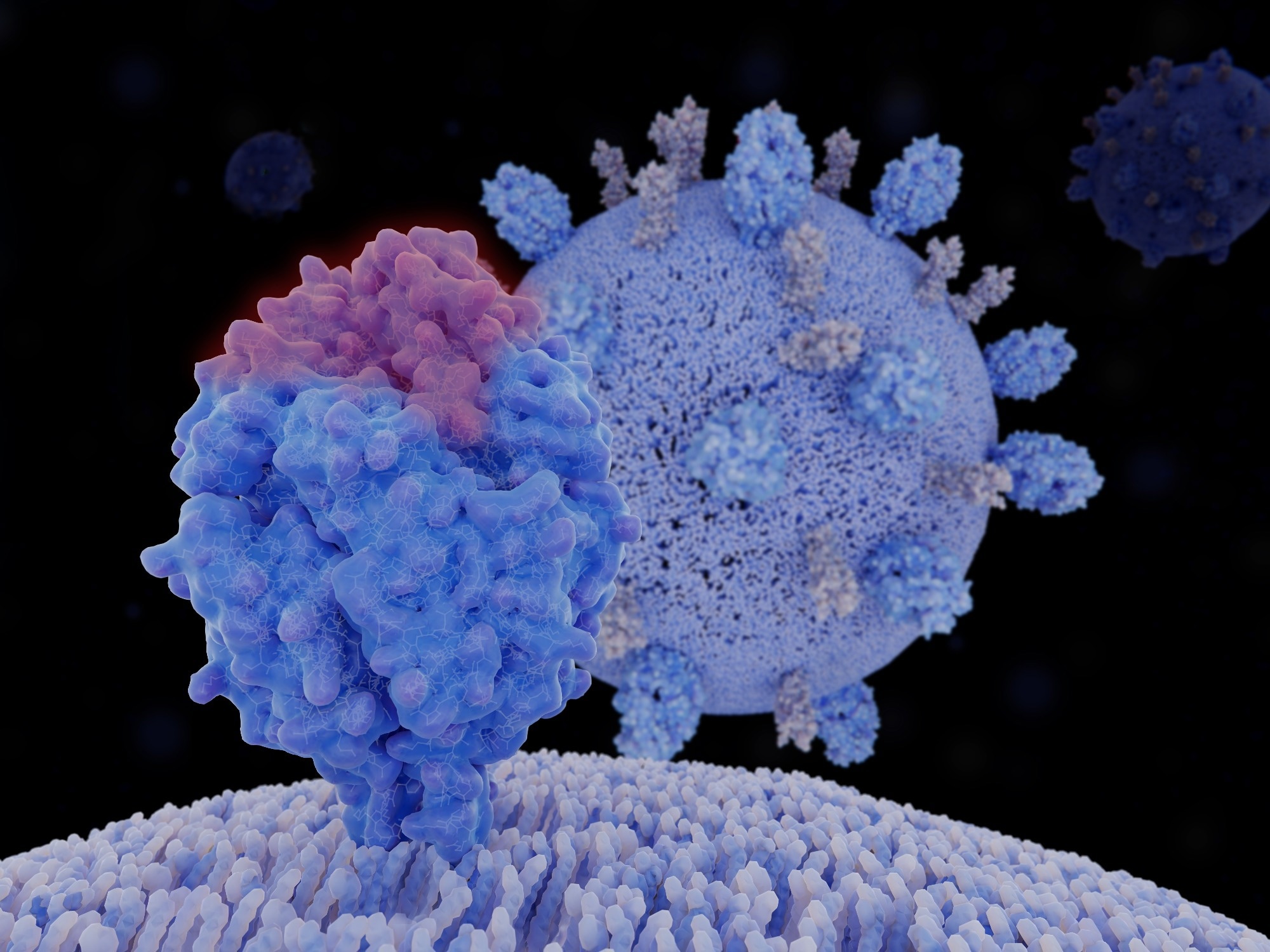 Image Credit: Juan Gaertner / Shutterstock.com
Image Credit: Juan Gaertner / Shutterstock.com
Supporting clinical data
A single intramuscular dose of nirsevimab consistently reduces clinically significant RSV outcomes while maintaining a safety profile comparable to placebo. In the phase III MELODY trial, healthy term and late-preterm infants aged 35 weeks or more received weight-based nirsevimab before the RSV season. As compared to placebo, nirsevimab reduced the rate of medically attended RSV-lower respiratory tract infection (LRTI) by 74.5%, as well as RSV-LRTI hospitalizations by 62.1%.3
During HARMONIE, a phase IIIb, pragmatic, and open-label trial, researchers assessed nirsevimab efficacy under routine-practice conditions in France, Germany, and the United Kingdom in over 8,000 infants 29 weeks’ gestational age or older entering their first RSV season. Nirsevimab reduced RSV-LRTI hospitalizations and very severe RSV-LRTI by 83.2% and 75.7%, respectively, with country-level efficacy against hospitalization of 89.6%, 74.2%, and 83.4% in France, Germany, and the U.K., respectively.4,5
In controlled studies, overall adverse-event rates were similar across groups, with most events considered mild to moderate, ranging from rash and fever to transient injection-site reactions. In the MEDLEY trial comprising high-risk/preterm infants, adverse-event incidences were similar to palivizumab.4,5
Policy and access
To date, nirsevimab has been approved in the European Union, the U.K., Canada, and the United States, with additional rollouts scheduled for Australia and other markets, reflecting a broadening global regulatory footprint.4,5 Public-health guidance has converged on protecting all babies during their first RSV season with a single dose, implemented either directly for the infant or through maternal vaccination, depending on country strategy.1,2,5
In practice, France and Spain adopted seasonal monoclonal antibody programs, whereas the U.K. implemented year-round protection with either nirsevimab or maternal RSV vaccination. The U.S. Centers for Disease Control and Prevention (CDC) recommended seasonal use of either option without preference. Taken together, these approaches aim to ensure that every infant is covered at the start of their first season.4,5
In the U.S., nirsevimab is listed in the Vaccines for Children (VFC) program, a unique classification for monoclonal antibodies. However, it remains the most expensive CDC-recommended childhood immunization, ranging from $395 to $495 USD/dose. Programs have urged operational fixes, such as bundling payments for birth-hospital administration and early financial support to clinics, to reduce financial barriers and enable timely dosing for infants born mid-season.5
During the 2023-2024 RSV season, U.S. VFC orders were temporarily suspended because of shortages, which were further complicated by the limited availability of the 100 mg dose. This led to interim guidance prioritizing higher-risk infants and pausing use in some older age groups.5
Importantly, these disruptions amplified inequities, with larger practices more likely to offer nirsevimab. Compared with practices with a greater proportion of publicly insured patients, those with a lower proportion were less likely to have nirsevimab available.5
Conclusions
Across clinical trials and real-world programs, nirsevimab consistently reduces medically attended RSV illness and hospitalizations with safety comparable to placebo, thereby extending protection to healthy term babies beyond traditional high-risk groups.3–5 Combining nirsevimab with maternal vaccination, while focusing its use in special populations and continuing genomic and safety surveillance, can sustain effectiveness, reduce disparities, and save lives.1,2,5
References
- Esposito, S., Abu Raya, B., Baraldi, E., et al. (2022). RSV prevention in all infants: which is the most preferable strategy? Frontiers in Immunology 13. DOI:10.3389/fimmu.2022.880368, https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2022.880368/full
- Sallam, M., Naji, H., Al Shibli, A., & Sallam, M. (2025). Maternal RSV vaccination to protect infants: current evidence and future directions. Exploration of Asthma & Allergy 3. DOI:10.37349/eaa.2025.100988, https://www.explorationpub.com/Journals/eaa/Article/100988
- Hammitt, L. L., Dagan, R., Yuan, Y., et al. (2022). Nirsevimab for prevention of RSV in healthy late-preterm and term infants. New England Journal of Medicine 386(9); 837-846. DOI:10.1056/NEJMoa2110275, https://www.nejm.org/doi/full/10.1056/NEJMoa2110275
- Drysdale, S. B., Cathie, K., Flamein, F., et al. (2023). Nirsevimab for prevention of hospitalizations due to RSV in infants. New England Journal of Medicine 389(26); 2425-2435. DOI:10.1056/NEJMoa2309189, https://www.nejm.org/doi/full/10.1056/NEJMoa2309189
- Wu, P.-P., & Ding, F.-R. (2025). Administration of Nirsevimab for RSV Prophylaxis in Infants: A Comprehensive Review. Vaccines 13(5). DOI:10.3390/vaccines13050470, https://www.mdpi.com/2076-393X/13/5/470
Further Reading
Last Updated: Nov 19, 2025