Ocular hypertension is a condition characterized by high internal pressure within the eye, which increases the risk of developing glaucoma.
 Tef | Shutterstock
Tef | Shutterstock
How is ocular hypertension diagnosed?
A diagnosis of ocular hypertension is primarily confirmed by examining the eye pressure. In order to do this, an ophthalmologist measures the pressure using an instrument called tonometer. A healthy eye pressure should be between 10 mm Hg and 21 mm Hg. Eye pressure measurements that are consistently above the upper limit are considered indicative of ocular hypertension.
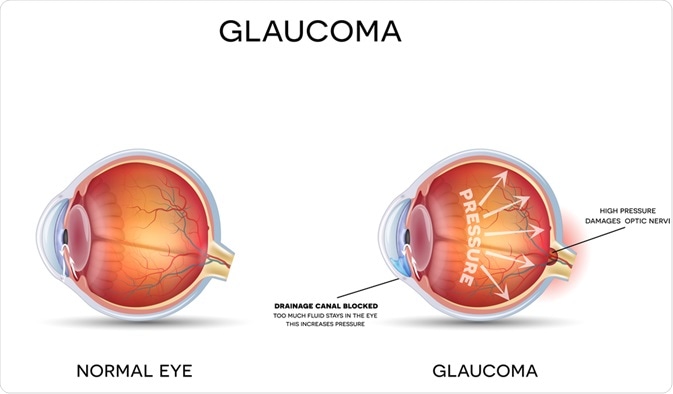
Since ocular hypertension significantly increases the risk of glaucoma, an ophthalmologist will also check the optic nerves for damage. Monitoring of the optic nerve is carried out using various imaging techniques, including Heidelberg retina tomography, a nerve fiber analyzer, or optical coherence tomography.
Finally, a visual field check will be conducted to check for any changes to the patient's peripheral vision, as glaucoma initially affects the peripheral or side vision, and may go unnoticed in its early stages. The most frequently used test is the Humphrey visual field test. In this method, a center fixation light and blinking test lights are used to check peripheral vision.
The patient should focus on the fixed light in the center and respond by pressing a button when blinking lights are noticed in the side vision. The patient must not move the eye to see the blinking light.
During the eye examination, gonioscopy can also be performed to check the internal drainage system of the eye. In this test, a gonioscope (a special contact lens prism) is used to investigate the angle formed between the cornea and iris of the eye. This angle defines the location from which aqueous humor flows out of the eye and enters into the venous system.
How is ocular hypertension treated?
Ocular hypertension is typically asymptomatic. Thus, it can remain undetected for a long time. Although ocular hypertension does not directly cause damage to the optic nerve or induce vision loss, about 10% of the people with high eye pressure eventually develop glaucoma. For this reason, a regular monitoring of eye pressure and screening for signs of glaucoma are important.
For patients with ocular hypertension (eye pressure ≥ 24 mmHg) who are at moderate to high risk of developing glaucoma (based on age, medical history, life expectancy, and personal preference) are prescribed eye drops to reduce intraocular pressure.
According to the Ocular Hypertension Treatment Study (OHTS), the treatment of ocular hypertension with topical medicines reduces the incidence of glaucoma by 50% to 60%.
A variety of eye drops are used to treat ocular hypertension. The most frequently used ones are prostaglandin analogs, which reduce the eye pressure by increasing fluid drainage. The second most commonly used medication is a beta blocker, which works by reducing the production of aqueous humor. In addition, alpha agonists, carbonic anhydrase inhibitors, and Rho kinase inhibitors are used as eye drop medicines.
In some cases, ophthalmologists also suggest selective laser trabeculoplasty (SLT) or argon laser trabeculoplasty (ALT) to reduce the elevated eye pressure. These surgeries are used when eye drops fail to reduce the pressure or cause adverse side-effects. Mechanistically, laser energy is applied to the eye’s drainage tissue to alter its chemical and biological properties and improve drainage.
Further Reading
Last Updated: Feb 28, 2019