The posterior cruciate ligament (PCL) is one of the important stabilizing ligaments of the knee joint, connecting the femur to the tibia, and it keeps the tibia from moving back on the femur.
Injuries to the PCL occur with powerful impact to the knee in a bent position, such as a person sitting in a car during a collision when the knee hits the dashboard or when a sportsman falls on a bent knee.
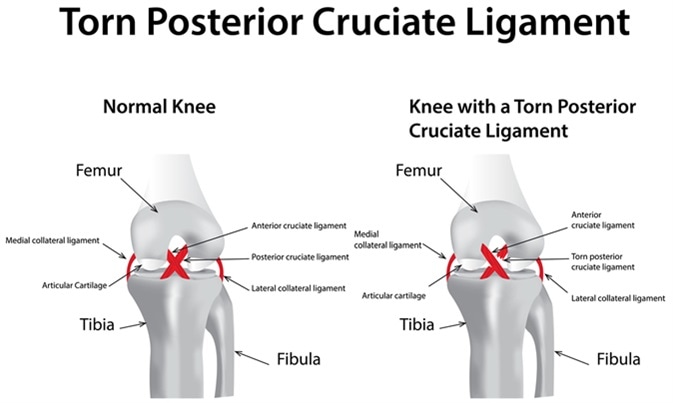
Torn Posterior Cruciate Ligament. Image Credit: joshya / Shutterstock
Anatomy
The knee is made of three bones, the femur, tibia and patella. These are held together by strong ligaments, the medial and lateral collateral ligaments, which prevent lateral knee movement, and the anterior and posterior cruciate ligaments, which keep the tibia from sliding too far forward and backward on the femur. The cruciate ligaments cross each other and are named for their insertion on the tibia. The PCL is tougher than the anterior cruciate ligament, and therefore is injured much less often. It is composed of two parts that join, making a structure about as thick as one’s little finger.
In most cases, PCL injury is accompanied by injuries to other knee joint structures.
Types of injury
PCL injuries may be strains or tears. Strains are graded into three categories based on the severity.
Causes
The PCL is injured by a high impact or undue torsion forces, such as:
- Direct collisions with the front of the knee joint
- Twisting motions
- Hyperextension of the knee
- A wrong step which results in any of the above
Symptoms
The symptoms of a PCL include:
- Pain accompanied by swelling which sets in almost at once after the injury – very often the pain is so mild as to escape evaluation, but is felt at the back of the knee and worsens when kneeling, and in front of the knee on running or when slowing down from a run
- Swelling and stiffness of the knee
- Onset of a limp with or without a feeling of giving way
- Difficulty in walking
A PCL injury is often followed by the development of osteoarthritis about 12-15 years later.
Diagnosis and Treatment
The diagnosis of PCL is made on the basis of the history as well as the symptoms and signs of the injury. The knee in such cases often ‘droops’ on flexion or may slide back excessively. Imaging tests such as X-rays or MRI are required if the diagnosis is not clear on examination or if the injury is older than three months. X-rays will also confirm avulsion fractures, while MRI scanning is preferred to evaluate soft tissue injury.
Treatment of such injuries is either surgical or non-surgical. Non-surgical treatment is preferred only for very recent injuries and consists of the R.I.C.E. approach (Rest, Ice application, Compression and Elevation). Knee braces may be used to stabilize the joint while the ligament is healing, and crutches will help take the load off the leg. Physical therapy will be prescribed once the joint inflammation goes down, with exercises to strengthen the muscles around the knee joint, prevent dislocations, strengthen the core muscles, and train in correct methods of twisting and stopping from a run.
Surgery is recommended for injuries to many parts of the knee joint simultaneously, and consists of reconstructing the ligament with a tissue graft from a specific tendon or from a cadaver. Several months of rest may be required before the new ligament fully grows along the graft to restore ligament strength. Arthroscopic surgery is preferred because of its relatively less invasive nature, shorter hospitalization periods, and faster recovery. Surgical treatment gives a better outcome in more active patients.
Physical therapy is an essential part of rehabilitation after PCL injury because it helps the patient to restore the fullest possible range of motion and strength to the knee. It usually begins once the swelling and pain recede, or about 1-4 weeks after surgery and may take several months to have the full desired effect.
Prevention
Prevention of PCL injuries includes:
- Proper warm up before any physically demanding activity
- Strengthening leg muscles
- Gradual increase in exercise intensity
- Use of supportive and comfortable shoes while doing physical activity
Further Reading
Last Updated: Jan 2, 2023