When a patient complains of joint pain, the first step is to identify the source of the pain: inflammatory or non-inflammatory. The next step is to establish the pattern of joint involvement. This includes the number of joints involved, the type of joints, symmetrical joint involvement, and onset of symptoms.
The third step is serologic testing to establish a diagnosis of seropositive or seronegative arthritis. Both PsA and OA are seronegative. Imaging studies are also helpful in differentiating different forms of the disease.
Differences Between Osteoarthritis and Psoriatic Arthritis
Osteoarthritis (OA) is a non-inflammatory arthritis. It is marked by the variable onset of symptoms and a wide range of severity. The joints are painful, but typically not warm or swollen. Morning stiffness is limited to less than an hour but joint pain worsens with activity and relieved by rest. Systemic symptoms are lacking, and there is no evidence of the involvement of other organs. The condition typically progresses without treatment.
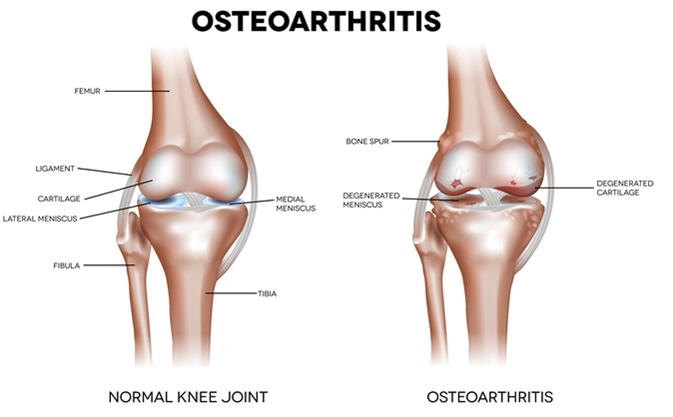
Knee Osteoarthritis and normal joint detailed anatomy. Image Credit: Tefi / Shutterstock
However, new modes of joint imaging such as arthroscopy, ultrasound and contrast MRI show that OA is also associated with significant inflammation in many patients. They may have morning stiffness for more than an hour and show marked joint swelling and bone erosions. This type of OA is called inflammatory OA and is difficult to distinguish from PsA, especially when the acute phase reactants are elevated and there is evidence of dysfunction of the synovio-entheseal complex. This could be due to fissure formation within the joint cartilage, fibrillation of cartilage and hypertrophy of cartilage cells, with the tendon insertions showing signs of micro-inflammation, possibly related to age.
Psoriatic arthritis (PsA) is an inflammatory arthritis presenting warm and swollen joints. Morning stiffness lasts for over an hour after waking up. Psoriatic skin lesions or ocular involvement are almost always present. The pain is not related to activity. The symptoms are typically relapsing in nature.
Etiology
OA was originally thought to be a result of joint degeneration by excessive use or loading of the joint. On the other hand, PsA is a complication of an auto-inflammatory process that also leads to psoriatic skin lesions. Both generalized forms of OA and PsA could be triggered in some cases at least by trauma or injuries to the joint or surrounding structures, even on a microscale.
Other factors that contribute to OA include obesity, aging, overuse by repeated movement at the same joint, and genetic factors. On the other hand, PsA is more commonly found to follow trauma, infections, certain medications, and stress, but genetic factors also play a marked role.
Pattern of Joint Involvement
OA of generalized type typically affects both small and large joints. Both OA and PsA have a characteristic predisposition for the DIP joints, the PIP joints, the knees and other large joints of the lower extremities. However, axial involvement is common in PsA, and begins with the cervical spine unlike ankylosing spondylitis, which it closely resembles, but which first involves the sacroiliac joints. Dactylitis is also characteristically found in PsA, but not in OA, though the latter does display PIP swelling due to inflammation of the tissues around the joint.
Enthesitis
Enthesitis is common to both conditions, but with somewhat different characteristics. In OA, early cases show thickening of the soft tissues of the joints, even before symptoms appear. Degenerative enthesitis is found as OA advances, and osteophytes appear, with narrowing of the joint space due to cartilage loss. Examination of joint fluid from OA patients typically reveals the presence of crystals that indicate degenerative bone changes not found in PsA.
On the other hand, PsA shows inflammatory enthesitis with diffuse bone edema being present on MRI.
In both conditions, the entheses may be the actual focus of early disease rather than the bone. In OA patients, the hand, for instance, may sometimes show thickening of the ligaments and other soft tissues before any bone involvement can be seen. In fact, this finding has led to a whole new category of OA, with cases that used to be classified as idiopathic being recognized as being due to enthesopathy. Patients with OA often develop lateral epicondylitis, enthesopathy of the calcaneum and bursitis of the greater trochanter, which are all forms of enthesopathy.
Age of Onset
Generalized OA typically begins after 50 years. It is more common in women because of the loss of estrogen with menopause. PsA also begins after this period in many cases but can begin much earlier or later.
Associated Changes
PsA is often associated with psoriatic dystrophy of the nails, and similar changes are more common in OA patients. These seem to be related to capillary elongation which leads to increased tortuosity.
Radiologic Signs
Plain X-rays show several differences between OA and PsA with respect to osteogenesis. OA patients show osteophytes and bone erosions which are para-articular and large. Enthesophytes are also seen at the peripheral joints and spine in OA. These tend to be flat. PsA patients, on the other hand, have syndesmophytes and features of periostitis.
PsA often shows signs of sacroiliac inflammation without any symptoms, though this is also seen in normal individuals.
Therapy
Non-steroidal anti-inflammatory drugs (NSAIDs) are used to relieve the pain in OA but are not very effective in PsA. Intra-articular steroids are useful over the short term in both conditions. While TNF inhibitors produce remission in a high percentage of PsA patients, they do not relieve symptoms to any significant extent in OA, but their use still slows the progression of joint erosive lesions.
Conclusion
While both OA and PsA can appear similar it is important to keep both in mind, particularly when the clinical response to a specific therapy is not as good as expected. This should lead to a re-evaluation of the grounds of the diagnosis so that better modes of treatment and therapies to prevent further bone destruction may be employed at earlier stages of the disease.
Further Reading
Last Updated: Feb 27, 2019