Introduction
Physiological response to meal skipping
Cognitive and behavioral effects
Impact on metabolic health
Skipping meals vs. intermittent fasting
Individual variability and risk factors
Clinical and public health implications
References
Further reading
Are skipped meals harmless, a metabolic shortcut, or a hidden health risk? Explore how the timing, structure, and frequency of meal omission can shape your metabolism, mood, and long-term well-being.
 Image Credit: grandbrothers / Shutterstock.com
Image Credit: grandbrothers / Shutterstock.com
Introduction
Meal skipping, whether deliberate through intermittent fasting (IF) or accidental amid hectic schedules, has become an increasingly common dietary pattern among adults. Epidemiological and experimental studies have confirmed that skipping breakfast, lunch, or dinner can alter glycemic control, appetite hormones, and energy balance; however, these findings remain inconsistent.
Thus, additional research is needed to compare how isolated and habitual meal omission influences subsequent food choices, diet quality, and metabolic risk. By clarifying the potential health benefits associated with this practice, clinicians can devise more accurate and evidence-based weight-management and nutrition guidelines.1
Physiological response to meal skipping
Skipping a meal leads to a rapid decline in glucose and insulin levels, which activates pancreatic α-cells to release glucagon into the bloodstream. To prevent hypoglycemia, glucagon acts on the liver to initiate glycogenolysis and gluconeogenesis to restore blood sugar levels.
As glycogen stores become exhausted, glucagon-driven lipolysis and the hypoleptinaemia-corticosterone axis replace carbohydrates with fat as an energy source. Thereafter, white-adipose triglycerides are hydrolyzed, hepatic acetyl-coenzyme A (CoA) levels rise, and ketone bodies become the brain’s alternative substrate.2,3
Concurrent hormonal shifts also occur, as leptin levels will quickly decline along with lower insulin levels, thereby activating the hypothalamic-pituitary-adrenal pathway and increasing cortisol levels. Systemic levels of ghrelin, an orexigenic stomach peptide, also rise during severe energy deprivation, which amplifies hunger signals and growth-hormone release while synergizing with leptin to promote fat mobilization.
Cognitive and behavioral effects
Skipping meals can transiently impact cognition, with several meta-analyses reporting weaker selective attention, poorer working-memory, and slower executive planning in binge-prone adults.
These observations have been similarly observed in rodents with intermittent high-fat or high-sugar access that exhibit object-recognition lapses during withdrawal phases. These rodents also become more irritable with more frequent mouth-boxing, biting and other aggressive responses after eight to nine weeks of alternate-day sugar exposure, with these behaviors similar to self-reported mood volatility in fasting individuals.
It remains unclear whether these disturbances persist; however, long-term spatial learning and memory typically remain intact. Patient outcomes may also vary with diet composition, sex, and baseline metabolic health, which suggests context-dependent recovery.4
Intermittent nutrient deprivation increases motivational “wanting” for palatable food, interferes with normal stress-induced appetite reductions, and accelerates compulsive food-seeking, even when energy needs are met. Once food becomes available, individuals or animals often consume larger, energy-dense meals to overcompensate for earlier deficits, which increases the risk of overeating and binge episodes.
Although short-term cognitive effects and irritability resolve quickly, the behavioral adaptations that protect blood glucose can inadvertently contribute to recurrent compensatory overeating over time, heightening chronic metabolic and mental strain.4
Impact on metabolic health
Cohort data suggests that limiting food intake to one or two structured meals aligns with lower body-mass index (BMI) values, while consuming snacks in addition to three meals each day predicts weight gain and a longer overnight fast strengthening this effect. In contrast, skipping breakfast and eating heavily at night promotes fat gain and hunger signalling.5
Insulin sensitivity is highest in the morning and lowest at night, with any meals consumed outside of this period increasing post-prandial insulin levels and impacting glucose control. Frequent small meals can reduce insulin levels under iso-caloric conditions; however, carbohydrate heavy snacks or those used to replace earlier meals do not confer the same benefits.
Several studies report that eating four to six times every day reduces total and low-density lipoprotein cholesterol, with this effects the result of insulin-driven hepatic synthesis and increased post-prandial reverse transport. However, low-frequency eating patterns are associated with poorly timed energy loads and poor lipid profiles.5
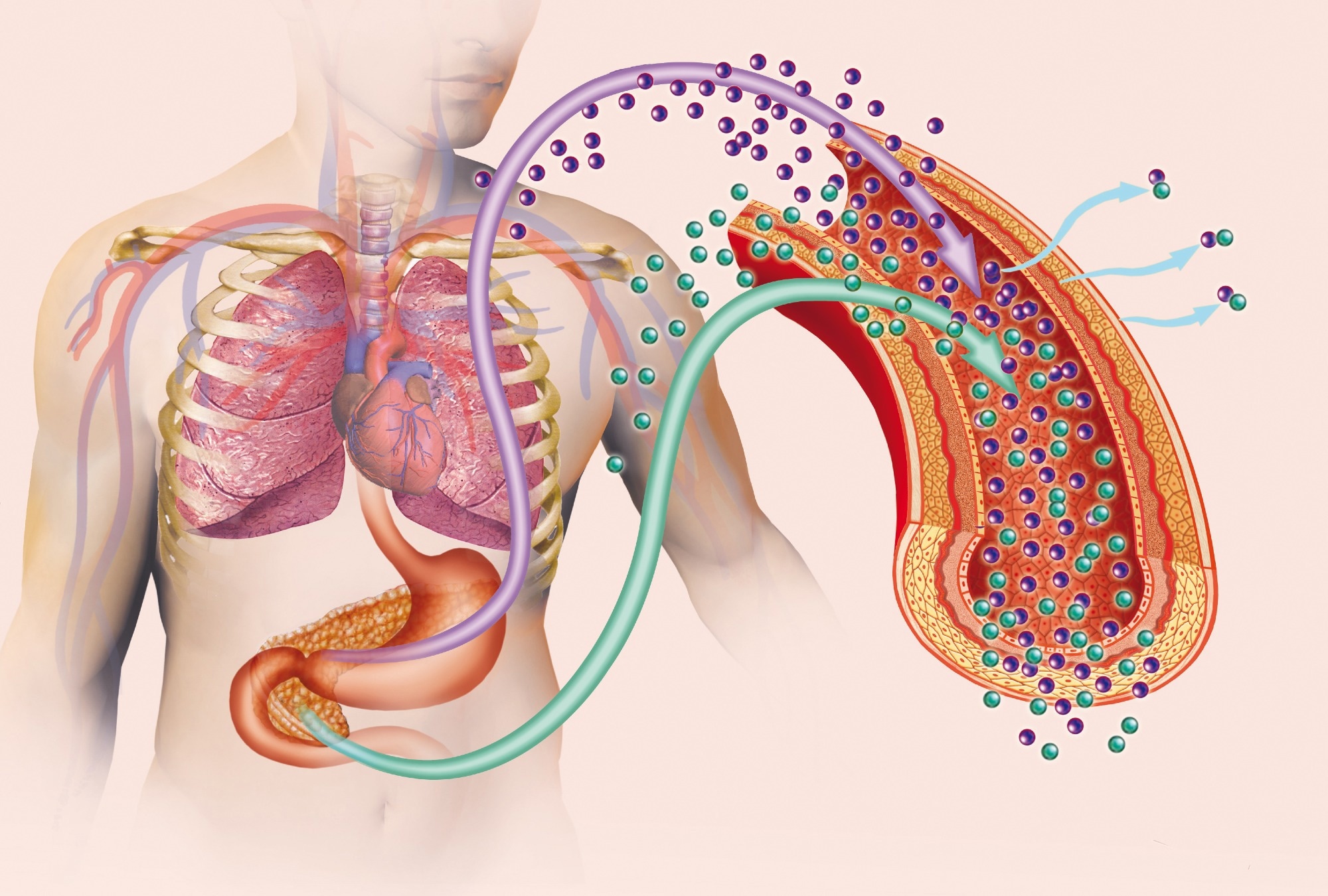 Image Credit: ilusmedical / Shutterstock.com
Image Credit: ilusmedical / Shutterstock.com
Skipping meals vs. intermittent fasting
Whereas skipping a meal lacks formal structure, intermittent fasting (IF) deliberately schedules periods of energy restriction and can be further practiced as time-restricted eating (TRE) or alternate-day fasting (ADF).
TRE limits total caloric intake to a four to 10-hour period during the day, thereby extending the nightly fasting phase without reducing weekly energy allowance. Comparatively, ADF alternates unrestricted food days with fast days limited to 25% or less of usual calories or complete abstinence.6
Both TRE and ADF can reduce body weight and fat mass by up to 14 % within three to 14 weeks. Modest improvements in triglyceride, high-density lipoprotein cholesterol (HDL-C), and fasting glycemic levels have also been observed; however, these benefits are similar to those associated with continuous energy restriction.
Meal skipping, which is usually studied as breakfast omission, remains unplanned and context-dependent. Prospective cohorts link habitual breakfast skipping to an increased risk of coronary heart disease and type 2 diabetes, with clinical trials reporting minimal weight change and inconsistent lipid effects over two to 16 weeks.
Intermittent Fasting: Transformational Technique | Cynthia Thurlow | TEDxGreenville
Individual variability and risk factors
Sex and age often determine chronotype, with children preferring early eating, teenagers frequently consuming meals later in the day, and older adults revert to morning schedules. Any disruption in daily eating patterns can desynchronize peripheral metabolic clocks desynchronise, as well as reduce insulin sensitivity and lipid clearance, especially after late-night eating.6
Recently, the European Prospective Investigation into Cancer and Nutrition (EPIC) calibration study reported that northern Europeans snacked more and ate most of their daily calories later in the day as compared to their Mediterranean peers. However, lower-income adolescents snack more frequently and gain more weight over time, linking socioeconomic status to risk trajectories. Thus, personalized guidance must consider these cultural and financial factors.6
Clinical and public health implications
In a previous Korean study, structured breakfast was associated with greater fiber, calcium, and potassium intake, as well as a more balanced macronutrient profile, whereas skipping breakfast lowered total energy and serum triglyceride (TG) levels. These observations suggest that regular and planned dietary eating patterns can be manipulated to support weight management or manage dyslipidaemia.7
One of the key limitations associated with skipping meals is an increased risk of micronutrient deficiency disorders. For example, among habitual skippers, 91% do not meet estimated average requirements for calcium levels, whereas 73% and 98% are deficient in vitamin C and folate, respectively. Skipping meals can also precipitate disordered eating patterns if individuals over-compensate at later meals with energy-dense foods.7
References
- Zeballos, E., & Todd, J. E. (2020). The effects of skipping a meal on daily energy intake and diet quality. Public health nutrition, 23(18), 3346-3355. DOI: 10.1017/S1368980020000683, https://www.cambridge.org/core/journals/public-health-nutrition/article/effects-of-skipping-a-meal-on-daily-energy-intake-and-diet-quality/89A963D23D416D25F7876094BD86C01E
- Zhang, J., Zheng, Y., Martens, L., & Pfeiffer, A. F. (2023). The regulation and secretion of glucagon in response to nutrient composition: unraveling their intricate mechanisms. Nutrients, 15(18), 3913. DOI: 10.3390/nu15183913, https://www.mdpi.com/2072-6643/15/18/3913
- Perry, R.J., Wang, Y., Cline, G.W., Song, J.D., Dufour, S., Zhang, X.M., Petersen, K.F. and Shulman, G.I. (2018). Leptin mediates a glucose-fatty acid cycle to maintain glucose homeostasis in starvation. Cell, 172(1), 234-248. DOI: 10.1016/j.cell.2017.12.001, https://www.sciencedirect.com/science/article/pii/S0092867417314435
- Rehn, S., Raymond, J. S., Boakes, R. A., Kendig, M. D., & Leenaars, C. H. (2025). Behavioural and physiological effects of binge eating: A systematic review and meta-analysis of animal models. Neuroscience & Biobehavioral Reviews, 106135. DOI: 10.1016/j.neubiorev.2025.106135, https://www.sciencedirect.com/science/article/pii/S0149763425001356?via%3Dihub
- Paoli, A., Tinsley, G., Bianco, A., & Moro, T. (2019). The influence of meal frequency and timing on health in humans: the role of fasting. Nutrients, 11(4), 719. DOI: 10.3390/nu11040719. https://www.mdpi.com/2072-6643/11/4/719
- Svendsen M, Forslund HB (2024) Meal patterns, including intermittent fasting - a scoping review for Nordic Nutrition Recommendations 2023. Food Nutr Res. DOI: 10.29219/fnr.v68.10505, https://foodandnutritionresearch.net/index.php/fnr/article/view/10505
- Min, C., Noh, H., Kang, Y.S., Sim, H.J., Baik, H.W., Song, W.O., Yoon, J., Park, Y.H. and Joung, H. (2011). Skipping breakfast is associated with diet quality and metabolic syndrome risk factors of adults. Nutrition research and practice, 5(5), 455-463. DOI: 10.4162/nrp.2011.5.5.455, https://e-nrp.org/DOIx.php?id=10.4162/nrp.2011.5.5.455
Further Reading
Last Updated: Jul 13, 2025