Introduction
Foundations of Speech Language Pathology (SLP)
Neurological basis of communication
Diagnostic tools and evaluation methods
Emerging therapies and technological advances
Current challenges and future research
References
Further reading
Speech-Language Pathology (SLP) is a clinical field that assesses, diagnoses, and treats communication and swallowing disorders across the lifespan. This article explores the neurological, technological, and social dimensions of SLP, highlighting emerging research and challenges.
 Image Credit: Prostock-studio / Shutterstock.com
Image Credit: Prostock-studio / Shutterstock.com
Introduction
Speech Language Pathology (SLP) is the clinical discipline devoted to assessing, diagnosing, and treating disorders of speech, language, voice, fluency, and swallowing. SLPs also play key roles in prevention, education, and advocacy for individuals with communication and swallowing needs. In addition to these responsibilities, SLPs are increasingly recognized as vital team members in highly specialized procedures such as awake brain surgery (ABS), where they assess and monitor language function intraoperatively, especially in pediatric populations. SLPs treat diverse patient populations ranging from infants with feeding difficulties and preschoolers mastering first words to adults regaining language after stroke, traumatic brain injury, head-and-neck cancer, or neurodegenerative disease.1
Foundations of Speech Language Pathology (SLP)
The American Speech Language Hearing Association (ASHA) states SLPs are experts in the areas of speech production, fluent timing, language form and content, cognitive-communication, voice and resonance, and feeding and swallowing. While SLPs are trained to screen for hearing issues and refer to audiologists, diagnosis and management of hearing disorders fall within the audiology scope of practice.
Speech disorders include those affecting how sounds are articulated and phonation is generated. Comparatively, language disorders affect the ability to understand or express meaning at the word, sentence, and/or discourse level. Communication disorders encompass any barrier to effective message exchange and may include speech, language, cognitive, voice, and/or swallowing issues.2
SLPs often construct individualized and evidence-based plans of care to maximize functional outcomes. Professional roles extend from prevention screening to complex rehabilitation, with practitioners working in neonatal intensive care units (NICUs), mainstream and special-education schools, outpatient clinics, acute hospitals, inpatient rehabilitation centers, long-term-care facilities, and clients’ homes. In hospital and rehabilitation settings, SLPs will frequently collaborate with registered nurses as well as physicians, occupational therapists, physical therapists, dietitians, and other allied health professionals to support tracheostomy management, stroke recovery, and dysphagia treatment. While SLPs and registered nurses (RNs) frequently collaborate, current research suggests there are relatively few formal studies on interprofessional collaboration in this area, highlighting a need for further research and implementation of structured interprofessional education and practice models.2
Neurological basis of communication
Broca’s area in the left inferior frontal gyrus of the brain constructs syntactically accurate utterances. Comparatively, Wernicke’s area, which is present in the posterior superior temporal cortex, decodes phonemes into meaningful language and relays this information to speech production centers.
These regions of the brain exchange information with each other through the arcuate fasciculus, a white-matter tract whose early-life myelination is essential for rapid repetition and phonological working memory. Damage to the arcuate fasciculus causes conduction aphasia.
The basal ganglia set speech rhythm and initiate well-timed articulatory movements, whereas the cerebellum calibrates rapid mouth- and tongue-muscle sequences for smooth delivery. The primary motor cortex subsequently executes refined commands to the orofacial musculature.3
When these nodes are injured or degenerate, characteristic communication disorders emerge. Large-artery stroke or traumatic brain injury often disrupts corticobulbar pathways, with up to 60% of patients experiencing dysarthria.
Hypokinetic dysarthria commonly affects people diagnosed with Parkinson’s disease, as basal-ganglia dopaminergic loss interferes with speech initiation and loudness. Neurodevelopmental conditions like autism spectrum disorder can also compromise social-pragmatic language and sometimes present with atypical cerebral lateralization.3
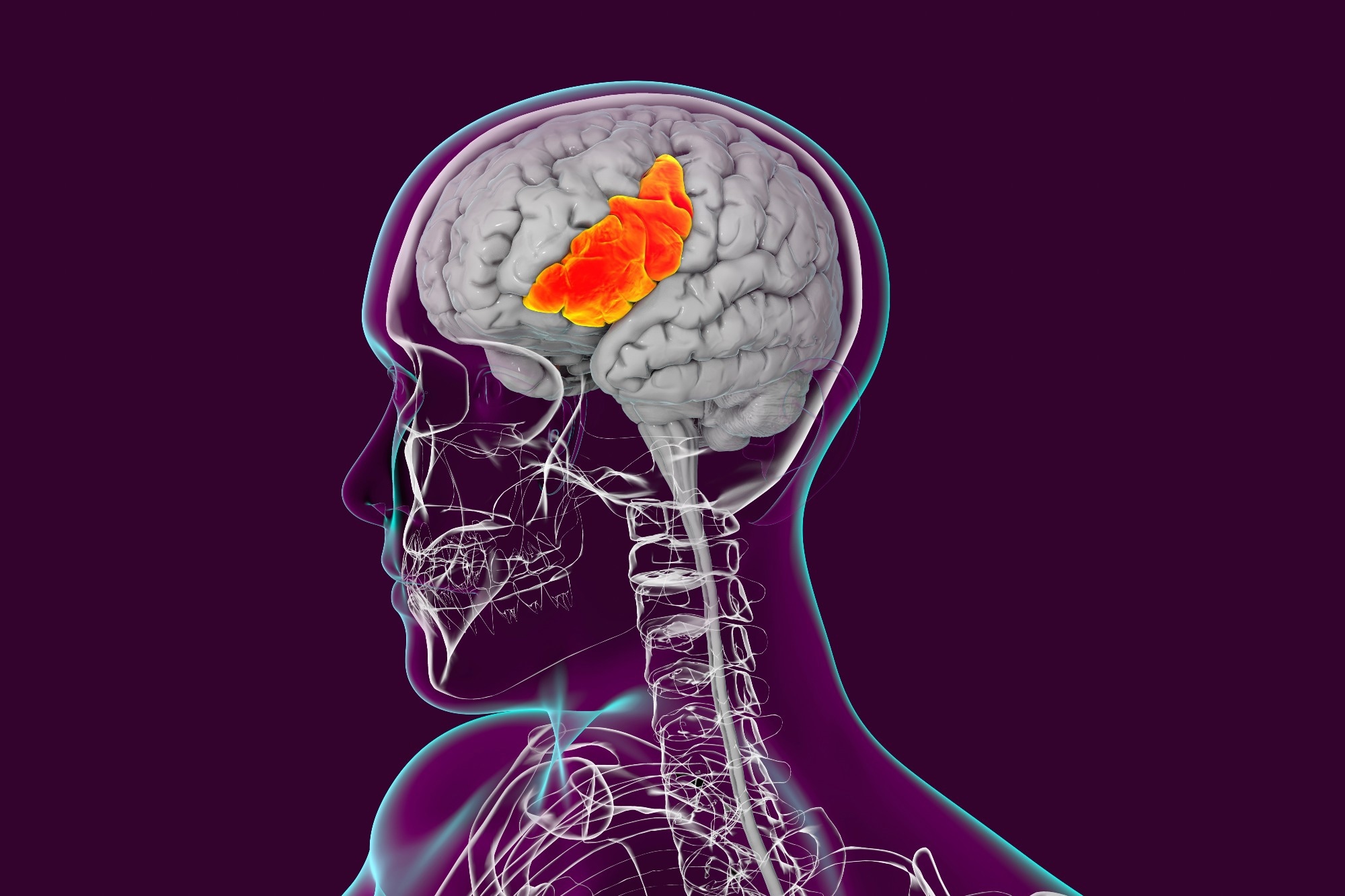 Image Credit: Kateryna Kon / Shutterstock.com
Image Credit: Kateryna Kon / Shutterstock.com
Functional magnetic resonance imaging (fMRI) has revealed coordinated bursts of motor planning, auditory feedback, and syntactic parsing during fluent speech. Conversely, lesion-symptom mapping of stroke survivors has identified the precise cortical voxels whose destruction impairs phonology, semantics, or speech timing. In young children, aberrant fMRI activation to speech predicts future language delay in autism, which exemplifies the diagnostic promise and ongoing research focus of neuroimaging.3
Effective communication is dependent upon the seamless dialogue of specialized cortical processors with motor-timing controllers. Understanding how discrete lesions, neurodegenerative processes, or developmental disorders disturb this dialogue can guide patient prognoses and targeted rehabilitation, from cerebellar timing therapies to basal-ganglia-focused pharmacology.3
Recent research also emphasizes the genetic underpinnings of many speech and language disorders, as well as the profound psychosocial impact (such as anxiety and depression) these conditions may have, highlighting the importance of holistic, individualized therapy that addresses biological, psychological, and social domains.3
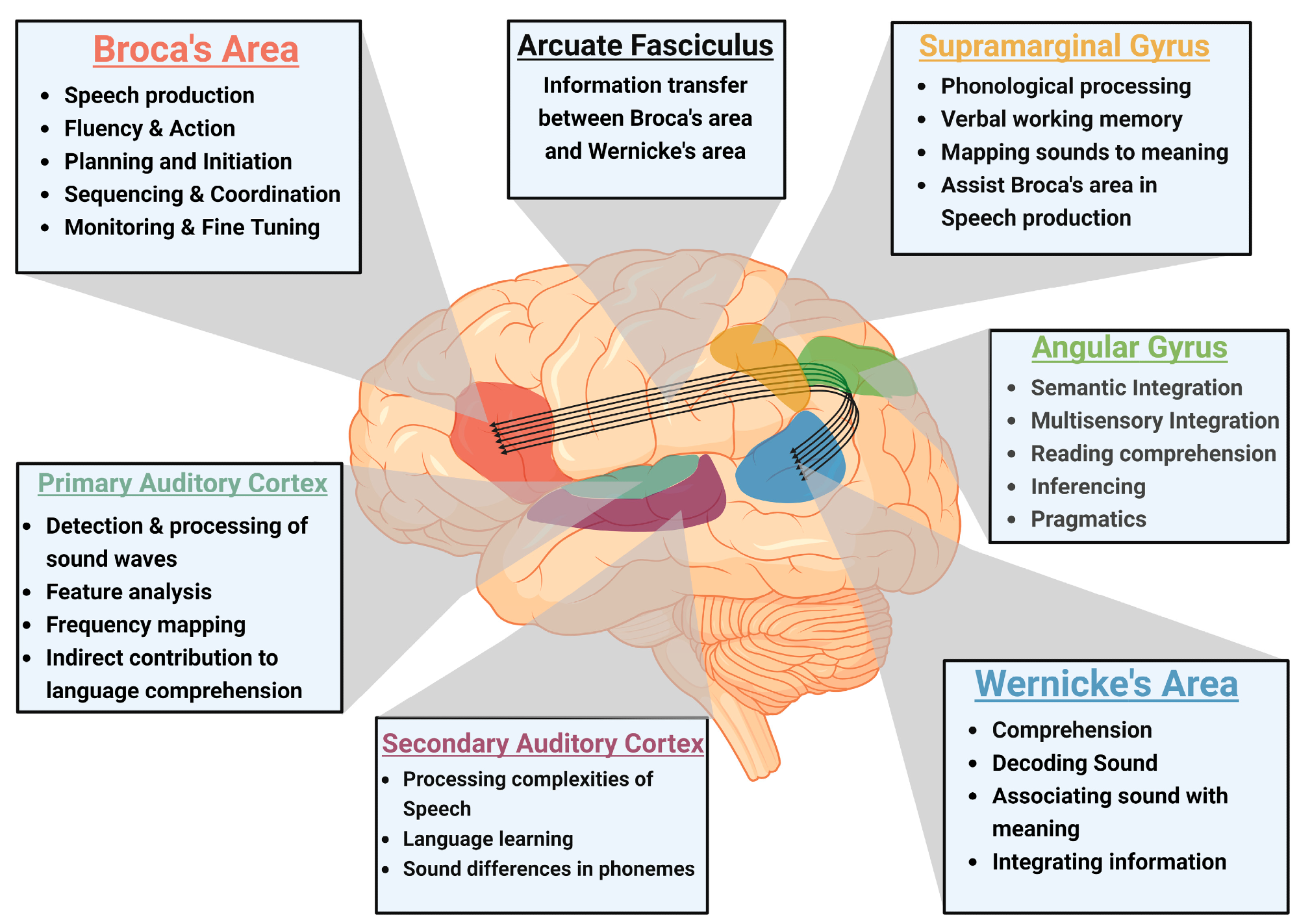 Neuroanatomy of language processing and speech production: The figure emphasizes the interconnected nature of Broca’s area, Wernicke’s area, and the Arcuate Fasciculus in speech production and comprehension. It also illustrates the supramarginal gyrus and angular gyrus, which are involved in phonological processing and semantic integration, along with the primary and secondary auditory cortex, responsible for auditory processing (figure created using BioRender).
Neuroanatomy of language processing and speech production: The figure emphasizes the interconnected nature of Broca’s area, Wernicke’s area, and the Arcuate Fasciculus in speech production and comprehension. It also illustrates the supramarginal gyrus and angular gyrus, which are involved in phonological processing and semantic integration, along with the primary and secondary auditory cortex, responsible for auditory processing (figure created using BioRender).
Diagnostic tools and evaluation methods
Standardized cognitive batteries, such as the Visual Short-Term Memory Binding Test (VSTMBT), Wisconsin Card Sorting Test (WCST), and Delis-Kaplan Executive Function System (D-KEFS), are used in select cases to assess specific cognitive skills related to communication. Most SLP evaluations rely primarily on behavioral and language-based assessments tailored to individual needs. Structured observational rating of daily functioning complements these tests to better inform treatment adjustments.
Structural and functional neuroimaging remains crucial, as MRI is used to assess regional atrophy and white-matter damage, whereas positron-emission tomography (PET) visualizes glucose metabolism and tau deposition to support differential diagnoses and prognoses.4
No single tool is definitive in diagnosing complex neurodegenerative or communication disorders; best practice is a multimodal, multidisciplinary assessment incorporating behavioral, neuropsychological, imaging, and biomarker data. Although machine learning and advanced neuroimaging are promising, their use is not yet universal in clinical practice, and cost, accessibility, and data integration remain barriers.4
Interpretation of these multimodal data streams occurs within multidisciplinary teams comprising clinicians, imaging specialists, neuroscientists, and data engineers to align both clinical and regulatory standards. Continuous refinement of these strategies through large harmonized datasets and machine-learning (ML) benchmarks is aimed at improving early detection, personalizing prognoses, and providing more equitable access to advanced diagnostics worldwide.4
Emerging therapies and technological advances
Emerging interventions include high-tech augmentative and alternative communication (AAC) devices, neuroplasticity-oriented protocols, artificial intelligence (AI)-driven personalization, and tele-enabled delivery. Modern AAC platforms integrate imaging, touch, mechanical, breath, and brain-computer interface access (BCI) routes to support flexible and portable speech generation while researchers work to reduce costs and complexity.
Intensive BCI training induces measurable cortical reorganization, thus highlighting the therapeutic potential of motor-imagery paradigms that utilize neuroplasticity to reopen communication channels. Parallel practice-based approaches, such as constraint-induced language and melodic intonation therapies, similarly strengthen residual language networks and complement device-based supports.5
AI and machine learning are equipped with word, message, and icon prediction, natural-language processing, and adaptive classifiers, all of which enable systems to learn individual patterns, reduce keystrokes, and broaden vocabulary access. Deep-learning algorithms further refine dysarthric speech recognition and improve BCI accuracy. It should be noted that many of these technologies are in development and not yet widely available in routine clinical care.5
Telehealth ecosystems embed AAC apps in smartphones and tablets to extend therapist oversight and real-time data sharing into homes and clinics. Mobile health dashboards similarly facilitate low-cost, continuous monitoring and a wider reach for remote speech therapy delivery. Despite rapid technological progress in AAC and AI-based solutions, barriers such as training requirements, cost, and device complexity continue to limit equitable access. Usability and user-centered design, including adaptation for different age groups and ability levels, are active areas of research and development.5
Ongoing research is investigating multilingual language models and cloud analytics to ensure that these innovations successfully translate from laboratory prototypes to daily rehabilitation contexts for users worldwide.5
Speech-Language Pathologist Career Video
Current challenges and future research
Long wait-lists, transportation barriers, and a shortage of first-language interpreters or multilingual providers, especially for rural or immigrant families, limit culturally competent care. Assessment and intervention practices may also vary widely across tools, service models, and documentation demands, which can lead to the uneven uptake of evidence-based methods.6
Service delivery for autistic children varies widely by setting, model, and clinician, with barriers such as funding, limited time, insufficient interprofessional collaboration, and community messaging identified as key obstacles. Supports include professional development, collaboration, and access to community resources.6
To date, most studies assume monolingual contexts; therefore, clearer definitions and robust trials are needed to understand foreign- and second-language outcomes for neurodivergent learners. Cultural and linguistic diversity are key considerations in the design and delivery of effective SLP services, and represent an ongoing area of research and advocacy. Practice-based research that actively involves families, clinicians, and policy makers in real-world service settings is increasingly advocated to bridge research-to-practice gaps.6,7
Since the available evidence base is dominated by children between the ages of six and 12 years, with only isolated adult cases, communication needs across the lifespan are largely unexplored. Beyond autism, conditions such as attention-deficit/hyperactivity disorder and intellectual disability receive little quantitative study and rely on small samples, thereby limiting their generalizability.7
In the area of neurodevelopmental disorders and foreign language learning, research highlights a diversity of intervention approaches (e.g., PECS, augmented/virtual reality, storytelling, gamification), but finds that most studies are small and not easily generalized. There remains a major gap in robust, large-scale research addressing the unique challenges of multilingual and neurodiverse learners.7
Pediatric SLP services in specialized contexts, such as awake brain surgery, face a lack of age-appropriate assessment tools and require further development of both resources and outcome tracking protocols.1
References
- Benabbou, N., Boutayeb, S., Chafik, K., Lafhal, H., Elhassani, M., & CHAFIK, K. (2025). Speech-Language Pathology Interventions in Pediatric Awake Brain Surgery: A Moroccan and Global Perspective. Cureus. 17(1). DOI:10.7759/cureus.77609, https://www.cureus.com/articles/306808-speech-language-pathology-interventions-in-pediatric-awake-brain-surgery-a-moroccan-and-global-perspective#!/
- Bloom, R. D., Tufano, V. E., & Perez, C. T. (2022). Registered nurses' and speech language pathologists' interprofessional collaboration: A systematic scoping review of the literature. In Nursing forum. 57(6). 1129-1136. DOI:10.1111/nuf.12802, https://onlinelibrary.wiley.com/doi/full/10.1111/nuf.12802
- Jaishankar, D., Raghuram, T., Raju, B. K., Swarna, D., Parekh, S., Chirmule, N., & Gujar, V. (2025). A Biopsychosocial Overview of Speech Disorders: Neuroanatomical, Genetic, and Environmental Insights. Biomedicines, 13(1). DOI:10.3390/biomedicines13010239, https://www.mdpi.com/2227-9059/13/1/239
- Shusharina, N., Yukhnenko, D., Botman, S., Sapunov, V., Savinov, V., Kamyshov, G., Sayapin, D. and Voznyuk, I. (2023). Modern methods of diagnostics and treatment of neurodegenerative diseases and depression. Diagnostics. 13(3). DOI:10.3390/diagnostics13030573, https://www.mdpi.com/2075-4418/13/3/573
- Elsahar, Y., Hu, S., Bouazza-Marouf, K., Kerr, D., & Mansor, A. (2019). Augmentative and Alternative Communication (AAC) Advances: A Review of Configurations for Individuals with a Speech Disability. Sensors. 19(8). DOI:10.3390/s19081911, https://www.mdpi.com/1424-8220/19/8/1911
- Binns, A. V., Cunningham, B. J., Andres, A., & Oram Cardy, J. (2022). Current practices, supports, and challenges in speech-language pathology service provision for autistic preschoolers. Autism & Developmental Language Impairments, 7. DOI:10.1177/23969415221120768, https://journals.sagepub.com/doi/10.1177/23969415221120768
- Andreou, G., & Argatzopoulou, A. (2025). Neurodevelopmental Disorders and Foreign Language Learning: A Systematic Review of Educational Interventions. Review Journal of Autism and Developmental Disorders, 1-10. DOI:10.1007/s40489-025-00512-2, https://link.springer.com/article/10.1007/s40489-025-00512-2
Further Reading
Last Updated: Aug 4, 2025