Adrenoleukodystrophy (ALD) is rare X-linked genetic disease that affects the adrenal glands (found on top of the kidneys) as well as the myelin in the brain and spinal cord. The incidence of ALD is approximately 1:20,000-50,000 people worldwide, affecting predominantly males.
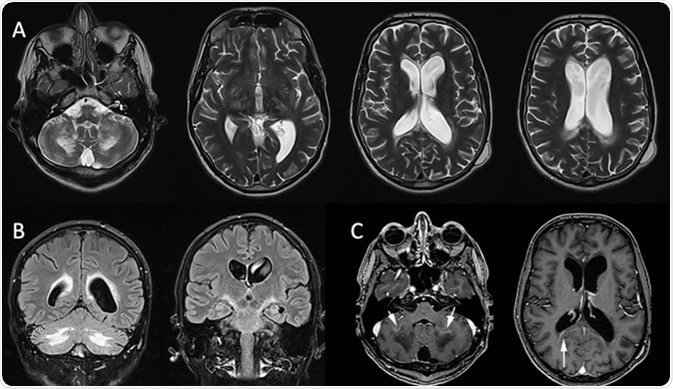
X-linked adrenoleukodystrophy: MRI in a 32-year-old man presenting psychiatric troubles and cerebellar ataxia two years ago. Axial T2-WI (A) and coronal FLAIR (B) show vasogenic edema involving the corpus callosum, the corticospinal tract and the cerebellar WM. Postcontrast Axial T1 (C) shows the inflammatory zone enhances (white arrow). Credit: Gilles Brun / Assistance Publique Hôpitaux de Marseille
There are 3 main types of ALD:
- Childhood Cerebral Adrenoleukodystrophy – most common form of ALD
- Adrenomyeloneuropathy (AMN) – adult form of ALD
- Addison Disease (Hypoadrenocorticism) – most males with ALD have Addison disease, but some rarer cases occur in which only the adrenal glands are affected (without nervous system defects)
Here, only childhood cerebral ALD will be discussed.
What are the Clinical Characteristics/Symptoms of ALD?
Symptoms vary according to the exact type and severity of ALD, and some symptoms may be apparent whereas others may not. Rarer forms of the disease carry additional set of symptoms not seen in classic childhood cerebral ALD.
What is Fight ALD?
In childhood cerebral ALD, the main symptoms are:
- Behavioural problems which begin during infancy – these include inability to pay attention or struggling mentally
- Neurological symptoms – some boys suffer from noticeable seizures before any cognitive symptoms begin
- Progressive symptoms include severe learning disabilities, ataxia (uncoordinated and often jerky movements), dysphagia (trouble swallowing), deafness and uncontrolled vomiting
- Adrenal insufficiency leads to abnormal metabolism with symptoms including a decreased appetite, darkening of the skin due to increased melanin production as well as muscle weakness and vomiting. Usually adrenaline and cortisol are affected, therefore affecting heart rate and blood pressure.
Further progression of symptoms tends to lead to a complete vegetative state (coma) within 5 years after nervous system symptoms present. In addition to these ‘classic’ or ‘set-1’ symptoms, around 5-10% of boys may also suffer from progressive paralysis of one side of the body (hemiparesis) and visual deficits. Dementia may also become apparent during adolescence, in addition to incontinence (uncontrolled urination), impotence (sexual dysfunction) and bowel issues.
The prognosis of childhood cerebral ALD depends on the severity, but due to its progressive nature, affected boys will often die within a few years after initial symptoms manifest. The other forms of ALD tend to be less severe and may live for a few decades, or live normal and full lifespans.
What Causes ALD?
ALD is caused by genetically inherited mutations to the ABCD1 gene. Normally, ABCD1 encodes the protein adrenoleukodystrophy protein (ALDP) which is involve in the transport of very long chain fatty acids (VLCFA) into cells to be degraded by peroxisomes or lysosomes.
Genetic mutations to ABCD1 result in a deficiency of ALDP, which leads to a build-up of VLCFAs within the blood and body tissues. The accumulation of VLCFAs is thought to be toxic to myelin in the nervous system and adrenal glands. Furthermore, VLCFAs can trigger neuroinflammation leading to the degeneration of myelin (like in multiple sclerosis).
How is ALD Treated?
ALD has no cure. However, depending on the severity and type, many of the features and symptoms can be carefully managed.
One common feature of adrenal gland dysfunction is adrenal insufficiency, where hormone levels are lowered. Long-term corticosteroid therapy can normalise hormonal levels, but there are many adverse effects of steroid therapy.
Alternative therapy by administration of Lorenzo’s oil, a natural combination of oleic acid (from rapeseed oil) and erucic acid (from olive oil), has been shown to modulate the build-up of VLCFAs and may potentially slow the progression of ALD. This is thought to be particularly useful for boys who have not yet presented with moderate symptoms of ALD; however, other studies have shown no significant effects. As with any alternative therapy, much more research is needed before any conclusions can be drawn.
Finally, recent clinical trials involving gene therapy to target mutated ABCD1 are currently underway and preliminary data is promising; however, this research is still in early phases.
Further Reading
Last Updated: Apr 9, 2019