Among young people, ocular injuries are common and comprise an important cause of preventable visual morbidity. Although ocular trauma is common, many injuries are minor and do not require hospital admission. However, it should be noted that certain ocular injuries are serious and potentially fatal. Certain forms of ocular trauma can manifest later as secondary glaucoma, also known as traumatic glaucoma.
Traumatic glaucoma is clinically defined as a post-traumatic rise in intraocular pressure (IOP) more than 21 mm Hg. Traumatic glaucoma can develop due to blunt trauma or injuries that bruise the eye; however, some forms are caused due to penetrating eye injuries. The development of the condition varies and may be acute or chronic in onset.
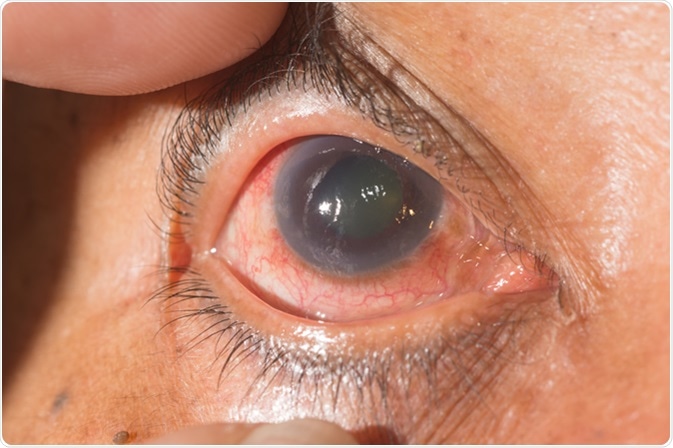
Close up of glaucoma during. Image credit: ARZTSAMUI / Shutterstock
What causes traumatic glaucoma?
Elevated IOP following trauma results from a multitude of factors. Drainage impairment may occur at the trabecular meshwork due to injury and hyphema, a pooling of blood inside the anterior chamber of the eye. Injury and inflammation to the lens or iris can also lead to the development of traumatic glaucoma.
Peripheral anterior synechiae (PAS) may also develop. These adhesions between the peripheral iris and the angular structures of the anterior chamber reduce outflow of aqueous humor (eye fluid), resulting in increased intraocular pressure.
Traumatic Glaucoma
What are the signs and symptoms of traumatic glaucoma?
- Aching pain in the eye – This may occur immediately after the injury
- Light sensitivity
- Blurred vision
- Blood collection (hyphema) and inflammation in the eye
- Elevated eye pressure –due to the blockage of the eye canals with blood and inflammatory cells
Pain may subside after the resolution of hyphema and inflammation, but the eye pressure may remain elevated. Although painless, increased IOP can cause significant damage to the optic nerve. The patient may remain asymptomatic for a long time until the visual loss has progressed to an advanced stage.
How is traumatic glaucoma diagnosed?
Doctors usually start by carrying out a complete eye examination to assess the extent of the damage. After confirming that the eye is not ruptured, the doctor examines the IOP and the angle structures.
The angle structures are measured using a slit lamp microscope and a gonioscope. Imaging can also be done performed with ultrasound biomicroscopy and optical coherence tomography (OCT).
If the optic nerve show signs of glaucoma, the following additional tests are carried out.
- Optic nerve thickness measurements
- Visual field testing and screening for early visual field loss
How is traumatic glaucoma treated?
The treatment goal for all forms of glaucoma is lowering IOP to less than 21 mm Hg. The pressure should be lowered in such a way that the optic nerve is not further damaged.
The treatment strategy for traumatic glaucoma includes a combination of pharmacologic agents with or without surgery.
Pharmacologic agents used to treat traumatic glaucoma include beta-blockers, prostaglandin analogues, alpha-adrenergic agonists, and carbonic anhydrase inhibitors.
Beta-blockers are the first choice agents. They decrease IOP by reducing the aqueous fluid inflow. Prostaglandin analogues relax the eye muscles and facilitate outflow of fluids, which, in turn, reduces IOP.
Alpha-adrenergic agonists and carbonic anhydrase inhibitors decrease the rate of aqueous humor production.
Steroids can help treat inflammation.
Surgery is considered when maximally tolerated medical therapy has failed and when the risk of progressive visual loss outweighs the risk of surgery. Argon laser trabeculoplasty, alternative laser procedures, and filtration surgery are possible surgical options.
If left untreated, traumatic glaucoma can cause permanent, irreversible damage to vision. Therefore, an eye examination is highly recommended following injury.
Further Reading
Last Updated: Feb 6, 2019