What is melatonin?
Melatonin in sleep regulation
Melatonin treatment in sleep disorders
Take-home message
References
Further reading
What is melatonin?
Melatonin is a hormone secreted by the pineal gland in response to darkness. The pineal gland, which is situated in the midline of the brain, analyses the current state of the environmental light-dark cycle and regulates the production and secretion of melatonin. 1 Exposure of the pineal gland to light inhibits the production of melatonin. 2
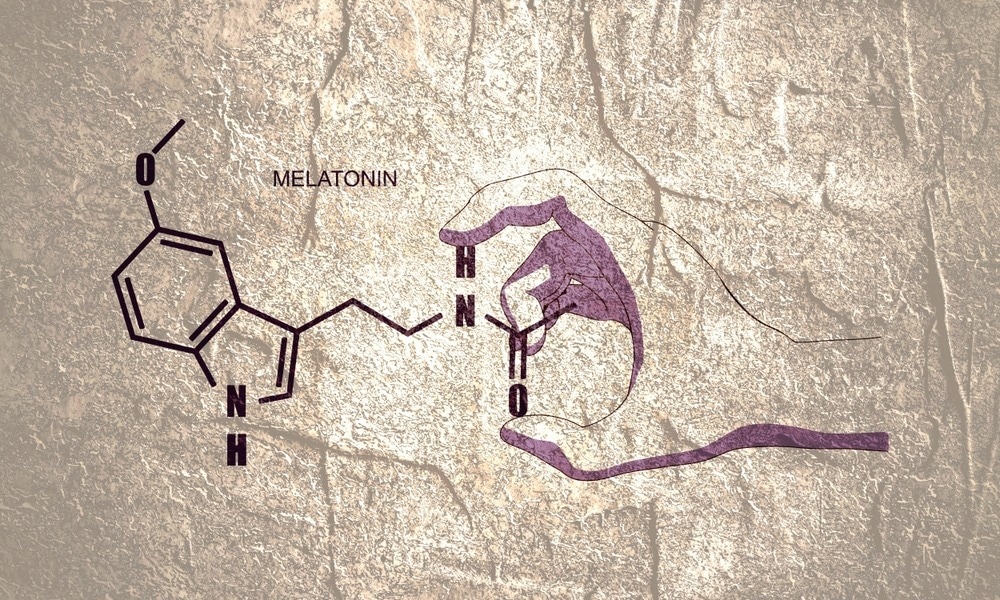
Image Credit: GrAl/Shutterstock.com
A cascade of enzymatic reactions takes place during the synthesis of melatonin. The first step is conversion of tryptophan to serotonin, followed by conversion of serotonin to N-acetylserotonin by the enzyme arylalkylamine N acetyltransferase and subsequent conversion of N-acetylserotonin to melatonin by the enzyme hydroxyl-indole-O-methyltransferase. 1
Although part of the brain, the pineal gland is situated outside the blood-brain barrier and gets signals through sympathetic innervation. The gland produces melatonin and releases it into the bloodstream without storing it. Melatonin can easily penetrate all body tissues and cross the blood-brain barrier to execute its functions. 1
Melatonin in sleep regulation
Sleep is a well-synchronized neurochemical process associated with many crucial physiological functions, including brain energy restoration, memory consolidation and extinction, and brain metabolite clearance. These functions are important for brain development, physical and mental well-being, and cognitive functioning. 3
Sleep has two distinct phases: rapid eye movement (REM) and non-rapid eye movement (NREM). These two phases periodically alternate throughout the night. NREM, also termed as slow wave sleep or deep sleep, is an indicative of sleep intensity. 4
The main function of melatonin is to regulate the circadian clock system and sleep cycle. 5 Suprachiasmatic nucleus (SCN), located in the hypothalamus, acts as the central pacemaker of the circadian system. The SCN synchronizes most circadian rhythms in the body, including sleep and wakefulness, temperature, feeding, and neuroendocrine and autonomic functions, with the 24-hour environmental day-night cycle. 4

Image Credit: aslysun/Shutterstock.com
Light acts as a primary stimulus to tune the SCN rhythm with the external environment. The neural output signal generated by the SCN induces the pineal gland to synthesize and release melatonin at night. Besides tuning the SCN, light inhibits melatonin synthesis. The influence of the environmental light-dark cycle on the pineal gland is responsible for a low plasma melatonin level at daytime and a high plasma melatonin level at night. 4
The most evident circadian rhythm is the sleep-wake cycle. Melatonin plays a crucial role in regulating sleep in humans. Sleep propensity (ability to transit from wakefulness to sleep) increases sharply at night two hours after the onset of melatonin synthesis in the pineal gland. 6
Melatonin also transmits information on night length to the brain and other organs, including the SCN, to maintain the sleep cycle. 6 The close association between circadian melatonin rhythm and sleep rhythm remains present in both normal and blind individuals. 7
Melatonin acts at the SCN to reduce the wake-promoting signal of the circadian clock. Melatonin also acts at the default mode network (DMN) regions in the brain to promote fatigue and sleep-like changes. 8
Melatonin’s action at the SCN is specifically mediated by two melatonin receptors MT1 and MT2. Studies on melatonin receptor knockout mice have shown that MT1 and MT2 receptors are associated with REM sleep and NREM sleep episodes, respectively. Melatonin regulates NREM sleep through its action on MT2 receptors present in reticular thalamic neurons. 9
Melatonin treatment in sleep disorders
Melatonin therapy is an effective intervention for a range of sleeping disorders. A significant proportion of individuals living with complete blindness develop non-24-hour sleep-wake disorder as they are not able to synchronize with the environmental day-night cycle. Administration of immediate release, as well as modified release melatonin preparations, have shown considerable efficacy in treating this disorder. 10
Clinically-approved melatonin receptor agonist tasimelteon has shown high efficacy in treating non‐24-hour sleep-wake disorder. This highlights the effectivity of melatonin receptor agonists in treating disorders associated with clock phase resetting. 11
Melatonin has shown high efficacy in advancing sleep onset and wake times to earlier hours and improving vigilance and cognitive functions in individuals with delayed sleep phase syndrome, which is a circadian rhythm sleep disorder characterized by sleep‐onset insomnia and difficulty in awakening at the desired time. 6
Insomnia is a common sleep disorder primarily observed in older people, particularly due to a reduction in melatonin production and secretion. Melatonin replacement therapies have been developed to replenish the deficiency of endogenous melatonin and treat such disorders. 4
Clinical trials involving insomnia patients aged 55 years and above have shown that prolonged-release melatonin formulations can effectively reduce sleep onset latency and improve sleep quality, morning alertness, and overall quality of life. 12
Children with autism spectrum disorder and other neurogenetic neurodevelopmental disorders also experience sleep disturbances. Recent evidence indicates that melatonin-based therapies, behavioral interventions, and parent education are the most effective approaches to mitigate sleep disturbances in these children. 13
What is melatonin -- and should you take it to fall asleep? | Sleeping with Science
Insomnia has a bidirectional association with nighttime hypertension, which can further increase the risk of cardiovascular disease and coronary heart disease. Poor sleep quality due to melatonin deficiency is considered a potential contributor to nighttime hypertension. 14
Prolonged-released melatonin formulations have proven efficacy in reducing systolic blood pressure at night in patients with nighttime hypertension. Melatonin also has considerable efficacy in improving sleep quality and quantity in hypertensive patients with sleep disorders. 15
Insomnia is significantly associated with Alzheimer’s disease (AD) and mild cognitive impairment (MCI). In addition to increasing the rate of cognitive decline in AD patients, insomnia can reduce the function of the glymphatic system, leading to decreased clearance and subsequent accumulation of AD-associated pathogenic proteins such as amyloid-beta. 3
Slow-release melatonin formulations have shown efficacy in improving sleep quality in AD patients. 16 AD patients treated with prolonged-release melatonin have shown significant improvement in cognitive functioning, such as memory and attention. 17
Take-home message
Exogenously administered melatonin can potentially improve non‐restorative sleep and circadian rhythm amplitudes and misalignments by reducing the activation of DMN. This mode of action of melatonin represents a promising investigational route for early intervention to promote healthy physical and mental aging.
References
1. Masters A, Pandi-Perumal SR, Seixas A, Girardin JL, McFarlane SI. Melatonin, the Hormone of Darkness: From Sleep Promotion to Ebola Treatment. Brain Disord Ther. 2014;4(1):1000151. doi:10.4172/2168-975X.1000151
2. Hardeland R. Chronobiology of Melatonin beyond the Feedback to the Suprachiasmatic Nucleus-Consequences to Melatonin Dysfunction. Int J Mol Sci. 2013;14(3):5817-5841. doi:10.3390/ijms14035817
3. Musiek ES, Holtzman DM. Mechanisms Linking Circadian Clocks, Sleep, and Neurodegeneration. Science. 2016;354(6315):1004-1008. doi:10.1126/science.aah4968
4. Zisapel N. New perspectives on the role of melatonin in human sleep, circadian rhythms and their regulation. Br J Pharmacol. 2018;175(16):3190-3199. doi:10.1111/bph.14116
5. Zhdanova IV. Melatonin. In: Aminoff MJ, Daroff RB, eds. Encyclopedia of the Neurological Sciences (Second Edition). Academic Press; 2014:1030-1033. doi:10.1016/B978-0-12-385157-4.00559-5
6. Zisapel N. Sleep and sleep disturbances: biological basis and clinical implications. Cell Mol Life Sci CMLS. 2007;64(10):1174-1186. doi:10.1007/s00018-007-6529-9
7. Zisapel N. Circadian rhythm sleep disorders: pathophysiology and potential approaches to management. CNS Drugs. 2001;15(4):311-328. doi:10.2165/00023210-200115040-00005
8. Gorfine T, Zisapel N. Late evening brain activation patterns and their relation to the internal biological time, melatonin, and homeostatic sleep debt. Hum Brain Mapp. 2007;30(2):541-552. doi:10.1002/hbm.20525
9. Cipolla-Neto J, Amaral FG do. Melatonin as a Hormone: New Physiological and Clinical Insights. Endocr Rev. 2018;39(6):990-1028. doi:10.1210/er.2018-00084
10. Emens JS, Eastman CI. Diagnosis and Treatment of Non-24-h Sleep-Wake Disorder in the Blind. Drugs. 2017;77(6):637-650. doi:10.1007/s40265-017-0707-3
11. Dhillon S, Clarke M. Tasimelteon: first global approval. Drugs. 2014;74(4):505-511. doi:10.1007/s40265-014-0200-1
12. Lemoine P, Zisapel N. Prolonged-release formulation of melatonin (Circadin) for the treatment of insomnia. Expert Opin Pharmacother. 2012;13(6):895-905. doi:10.1517/14656566.2012.667076
13. Tordjman S, Najjar I, Bellissant E, et al. Advances in the research of melatonin in autism spectrum disorders: literature review and new perspectives. Int J Mol Sci. 2013;14(10):20508-20542. doi:10.3390/ijms141020508
14. Roth T. Comorbid insomnia: current directions and future challenges. Am J Manag Care. 2009;15 Suppl:S6-13.
15. Grossman E, Laudon M, Zisapel N. Effect of melatonin on nocturnal blood pressure: meta-analysis of randomized controlled trials. Vasc Health Risk Manag. 2011;7:577-584. doi:10.2147/VHRM.S24603
16. Singer C, Tractenberg RE, Kaye J, et al. A multicenter, placebo-controlled trial of melatonin for sleep disturbance in Alzheimer’s disease. Sleep. 2003;26(7):893-901. doi:10.1093/sleep/26.7.893
17. Wade AG, Farmer M, Harari G, et al. Add-on prolonged-release melatonin for cognitive function and sleep in mild to moderate Alzheimer’s disease: a 6-month, randomized, placebo-controlled, multicenter trial. Clin Interv Aging. 2014;9:947-961. doi:10.2147/CIA.S65625
Further Reading
Last Updated: May 10, 2024