An interview with Steven Lazer, Global Healthcare CTO, Dell Technologies Health and Life Sciences
Digital pathology is a powerful new tool to help enhance pathology worldwide and requires a lot of data. Please give an overview of the data involved and how you are involved in your role at Dell EMC Life Sciences?
Digital pathology is the viewing, analyzing, and managing of digitalized pathology slides with computer technology called whole slide imaging, or WSI, which generates a tremendous volume of data. A single whole slide image can be a gigabyte or larger in size.
Image credit: Huron Digital Pathology.
Since AI applied to digital pathology is a relatively new endeavor for most US healthcare systems, it is our role to provide strategic guidance on how to accommodate storage needs within the IT budget and operational requirements.
Additionally, as we begin to see the research and clinical value in historical pathology slides evolve, we must provide the ability to unlock this rich vault of data in a simplified and cost-effective manner. Our history in managing large data sets of imaging and EMR data allows the team to develop high-performance architectures to support the analysis of this data.
In my opinion, the biggest challenges facing IT as digital pathology becomes mainstream, are:
- Providing expandable storage: A single slide captured by a WSI scanner can generate a vast amount of data. Multiply that by hundreds of slides imaged per day, and it’s clear why expandable capacity is required to maintain the ever-growing repository of historical image data.
- Bringing intelligence to unstructured data: On its own, the digital image of a scan is not much more useful than the physical slide. For an image to have value, it needs to be ingested into a structured system—with fast access for collaborative purposes. This involves the creation of hundreds of annotated tags to go with the image, requiring high-performance computing power and AI-enhanced processing. This metadata, along with medical notes, must be combined with the digital images and placed together into object storage and attached to the patient’s electronic medical record (EMR).
- Accessible anywhere, anytime: Digital pathology image data and its tags need to be accessible within the local healthcare facility and across the wider medical community for primary diagnosis, remote consults via telepathology, and virtual peer review for difficult-to-diagnose cases and clinical trials, education, as well as research. When these images are integrated with a laboratory information system (LIS), an EMR, and other systems, this approach ensures data portability for a complete patient view. The challenge is to do this effectively and securely in a multi-cloud environment.
Huron Scan Index Search
What have we learned from other imaging modalities that can be applied to pathology as it moves to digital?
Advancements in other imaging modalities have already had an impact on detection, diagnosis and treatment of a variety of diseases – leading to an evolution in the standards of care. Continued growth of MRI and other imaging innovations have led to an explosion of digital imaging data which includes 3D and virtual reality, intra-operative, nuclear, and portable imaging.
The healthcare industry has undergone significant consolidation – especially in the U.S. – which has led to an increased need for integrated systems. This requires centralized data repositories, like the vendor-neutral VNA, and interoperability with other information systems. On top of the raw data being captured AI and advanced analytics are being used to mine and to promote the “interesting data” contained in the images.
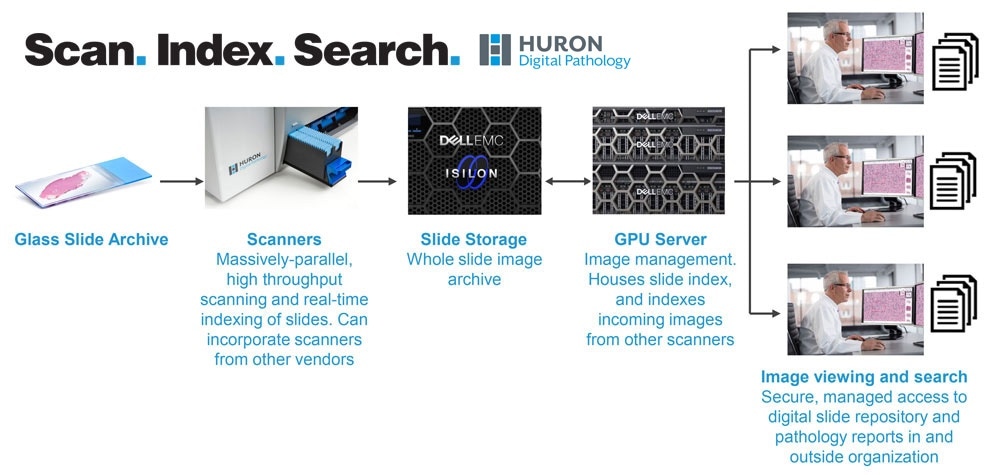
Image credit: Huron Digital Pathology.
Although financially impractical, images are generally retained forever. However, in general, it’s widely agreed upon that an intelligent imaging retention strategy is important. A well thought out data management strategy will make it possible to define a performant, regulatory compliant architecture with the ability to scale out and up as needed.
What is unique about pathology compared to, say, radiology, from an IT perspective?
We have learned a tremendous amount in dealing with traditional radiology imaging data sets. However, elements such as data gravity were a minimal concern. With digital pathology, the data sets are so large we need to invent new ways to provide agility with the data. In digital pathology, clinical decisions could have significant treatment impact on patients, but tumor boards, for example, still rely heavily on a less methodical approach than those followed by radiologists.
Even though most specialties are experiencing shortages, there is a severe global scarcity of pathologists1, especially in pathology subspecialties. This means that the need to move to digital pathology is even more pronounced, but harder to execute due to limited capacity for training in pathology departments.
Unlike radiology, where images were improved through 3D technology and algorithms removing artifacts, digital pathology offers the potential to introduce entirely new types of machine analysis of pathology slides. This could lead to faster and more accurate diagnoses, leading to improved care for the patient. We are seeing emerging technologies created for things like slide over-reads to validate quality standards.
Utilizing the AI tool sets we can apply to digital pathology, we can improve the standard of care as we reduce the workload of pathologists helping them to focus their time on the cases requiring their attention. The impact on existing workflow is very different. For radiology, the specialty was entirely image-based, so moving to digital was a natural step that fit within the existing workflow. In digital pathology, however, it requires adopting an extra step, and fundamentally changes the workflow.
With the larger scale of the data sets and the desire to apply AI and high performance compute (HPC) to those data sets the communication networking of the digital pathology ecosystem of devices may impact other workloads on the network. High performance (10Gb minimum) software defined networking will minimize data flow impacts. The ability to segment the data streams and dynamically manage the network will offer the best possible solution to manage the impact of the large data streams.
How are new artificial intelligence techniques impacting how IT infrastructure companies serve hospitals?
AI techniques are requiring healthcare providers to modernize their IT architecture. This includes:
- High performance modern data platforms: To house both structured and unstructured data platforms that can accept a variety of images, video and other contemporary media.
- Multi-cloud evolution: The increasing availability of hosted cloud platforms and the growing importance of matching workload requirements to the storage location.
- Next-generation applications: More efficient image viewing and data management technologies.
- Big data and analytics: The maturation of data lake technology and the optimal use of big data analytics algorithms.
- AI capabilities to support the learning algorithms being developed.
- Weightless methodologies to exchange data between physical locations.
- The ability to provide AI capabilities at the point of data collection.
Having this in place will enable digital pathology workflows and allow healthcare organizations to work with research and biopharma companies to develop and apply algorithms that harness the advances in computer vision, machine learning, and artificial intelligence to augment clinical diagnosis.
How do you think Digital Pathology will coexist in with PACS and Enterprise Imaging?
Due to the level of maturity in radiology PACS and consolidation in the industry, IT departments are now looking at “archive neutral vendors”, not to be confused with Vendor Neutral Archives or VNAs, as there will be a need for archives of different uses. Some people also refer to it as VNA 2.0. These archives will need to be ready to support multiple workflows, incorporate the most recent interoperability standards, like IHE IL7, and be ready for a step-function increase in processing requirements to enable AI in the future.
If done correctly, a lot of clinical specialty areas can be supported using a fully integrated VNA – radiology, cardiology, pathology, and more.
What the most exciting developments you are seeing as pathology becomes digital?
Digital pathology has been around for a while. However, just recently have we began seeing FDA approvals of some clinical tools. Additionally, significant progress has been made with healthcare applications of AI. The journey towards applying AI in mainstream decision-support tools is now well underway and we expect to see many additional AI-based applications in healthcare – with a significant impact expected on the efficiency of decision-making based on the clinical outcomes to date.
One of the ripest opportunities to improve standard-of-care by is by augmenting pathologist diagnoses with other forms of data such as genomics and merging the data sets. Algorithms are still evolving, but digital pathology applications in AI are already leading to the democratization of pathology by helping it evolve from art to science – ultimately impacting patient care for the better. New technologies will come forward to speed search and comparative capabilities combined with AI functions to infer diagnoses, but will require the pathologist to be the final point of decision in patient care.
One of the most exciting developments is a partnership with Huron Digital Pathology and Dell Technologies to bring intelligence to the unstructured data through image search – connecting pathologists to the vast knowledge contained in pathology reports on a real-time basis.
What is the future of digital pathology from an IT perspective?
The future digital pathology as an IT solution will encompass several things:
- Flexible, scalable storage for large volumes of data:
- IT departments need high-capacity storage platforms for structured and unstructured data that can grow dynamically as image data is supplied by WSI scanners.
- Research utilizing whole slide imaging data needs to be located, provisioned, and executed quickly, with the ability to identify specific data sets by any number of demographic parameters such as patient name, disease type, date, or serial number.
- Adding intelligence to this pool of unstructured data will help to unlock the true value of the data
- High-performance networks need to transmit the large data sets in near real-time from the point of generation
- By utilizing micro-segmented networks, we can segregate the data communications to allow dedicated pathways for the data streams.
- High-performance compute (HPC) for fast data indexing
- An HPC platform to accelerate the indexing of large WSI datasets for fast retrieval, and servers with shared computing power for intensive workloads such as clinical trials and AI-enabled drug discovery.
- Advanced analytics for meaningful insights
- IT departments need a platform that can provide a basis for data analytics to help unlock the value that exists within pathology and other medical data.
- Multi-cloud integration for collaboration
- Provide flexible access for telepathology and teleconsultation to indexed WSI data via hybrid cloud options, enabling multi-tenant integration across all your private, hybrid, and public cloud services.
- All this needs to be done within a cloud networking and security framework that allows organizations to confidently embrace and work across multiple clouds.
- IT solutions built for interoperability
- Migrate to open, free and publicly available digital imaging and communications in medicine (DICOM) format.
- The DICOM data format is the standard of other imaging modalities in HCLS today.
- There is a big push in pathology to convert everything over to DICOM, and to do it at the scanner level right from the start, not in the software after the fact.
- Leverage industry-wide global standardization
- Proprietary data solutions will limit the portability of patient data.
- Partner through standards, labs and open software foundations to limit future vendor lock-in.
Where can readers find more information?
About Steven Lazer
Steven Lazer is the Global Healthcare CTO for Dell Technologies Healthcare & Life Sciences. He concentrates on translating health organizational requirements into best-practice IT strategies that deliver accelerated Health IT ecosystem implementations – focusing on Independent Software Vendor (ISV) partnerships, Electronic Medical Record (EMR) implementations and development of cloud-based solutions.
Prior to his CTO role, Steven spent 5 years as Sr. Technology Consultant and Advisory Solution Engineer in Dell EMC. Steven has over 20 years of experience in Health IT production environments and more than 30 years in IT, with over 200 successful EMR implementations.
Recent roles before joining Dell Technologies include Director of Technical Services at North Memorial Health Care (an early Epic adopter) and Principal Consultant at Midwave Corporation (an IT consulting firm now acquired by Datalink Corporation). Steven is a Technology Advisor with ECare21 – a company developing a mobile virtual care platform for chronic care management and remote patient monitoring.
Sources:
- Severe shortage of pathologists and laboratory services
US (*)
- 2010: 17,986 pathologists
- 2015: 15,000 demand
- 2025: 25,000 predicted
Hong Kong (**)
- 1 pathologist for 26,500 people
Singapore (**)
- 1 pathologist for 48,900 people
Malaysia (**)
- 1 pathologist for 103,000 people
Fewer than 2% of medical graduates choose to pursue pathology2
Sources: (*) College of American Pathologists / (**) Global Healthcare Technology article ‘Pathology’s workforce crisis - impact on acute healthcare in Australia’
1. Facts and Figures on Cancer in 2019, American Cancer Society, 2. The First Frontier for Medical AI is the Pathology Lab, IEEE SPECTRUM, Nov 28, 2018