The early part of this year saw the reports of the first cases of COVID-19 in China’s Wuhan City. Within six months, it had spread to almost every country across all borders, causing more nearly 11 million cases and over 519,000 deaths. Now, a new study by researchers at Yale University and published on the preprint server medRxiv* reports on the plasma levels of biomolecules that reflect vascular damage in COVID-19.
The disease caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) is primarily a respiratory illness, with a significant minority of patients developing acute respiratory distress syndrome (ARDS), often ending in multi-organ dysfunction and death. However, the underlying disease process which decides how and at what pace clinical features progress or worsen is unknown, even with so many millions of cases.
Indeed, multiple biomarkers of endotheliopathy segregate with increased mortality. While a number of biomarkers, including D-dimer, troponin, and B-type natriuretic peptide, have been associated with survival in COVID-19, there is currently a paucity of vascular-specific biomarkers that can help prognosticate patients with COVID-19. This is a critical unmet need, given the emerging evidence for endothelial cell involvement in COVID-19 pathogenesis. Development of circulating markers that can detect specific aspects of COVID- 19 pathogenesis may be critical to guide the use of novel therapeutic strategies, including those that may safeguard the vasculature, such as dipyridamole or inhibitors of the complement cascade. Further validation of our findings in larger patient cohorts, together with mechanistic studies to understand the causes of endothelial injury and its consequences for immune activation, vascular dysfunction, and thrombosis, promise to provide pivotal insights into COVID-19 pathogenesis and guide clinical management.

 This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
Endothelial Damage in COVID-19
Earlier studies have shown that patients with cardiovascular disease have poor outcomes compared to other COVID-19 patients. Autopsy findings in these patients show endothelial damage and the formation of new blood vessels. However, there is no reliable description of the circulating vascular markers that predict the severity of disease and mortality.
The current study aimed to understand how factors associated with vascular health are released in a series of COVID-19 patients admitted to a single-center, the Yale-New Haven Hospital. All had diagnoses confirmed by reverse transcriptase-polymerase chain reaction (RT-PCR).
The researchers say their findings “demonstrate a significant increase in markers of angiogenesis and endotheliopathy in patients hospitalized with COVID-19.”
The Study: Evaluating Vascular Markers
The researchers collected blood from 40 critically ill patients between April 13 and April 24, 2020. All these patients were admitted to the intensive care unit (ICU) at the time of sampling. There were also 9 non-critical patients. All were diagnosed to have COVID-19.
They also drew blood from another 13 asymptomatic healthy patients as controls. The subjects were all followed up until May 23, 2020, when 12 of the 40 critically ill patients had died, and 25 were discharged, as well as all the less ill patients, none of whom had progressed in severity of illness. The remaining 3 were still hospitalized.
Blood was tested for markers of new blood vessel formation and epitheliopathy. Comparing protein levels in the three groups of subjects, namely, ICU vs. non-ICU patients, non-ICU patients vs. controls, and ICU patients who died vs. ICU survivors.
The Findings: Higher Vascular Injury Markers in COVID-19
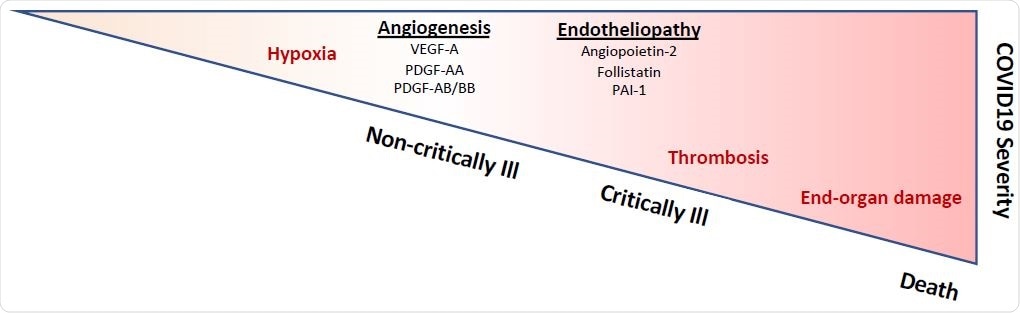
The researchers came to three conclusions. There were several circulating factors like VEGF-A, PDGF-AA, and PDGF-AB/BB, which encourage angiogenesis, present at markedly higher levels in the non-ICU patients compared to controls. This may be one contributor to the vascular remodeling seen in this condition.
The second finding was the increased level of angiopoietin-2, FLT-3L, and PAI-1, in ICU patients, showing the presence of endothelial damage. This agrees with new data that reflects endothelial involvement in critical disease. Other markers of angiogenesis and endothelial function are not raised or only mildly so.
The third related to survival and showed that the increase in markers of endothelial vascular damage was clustered with in-hospital mortality. In other words, the endothelial injury could predict mortality in COVID-19.
The investigators sum up: “Overall, we have identified a panel of circulating markers associated with angiogenesis and epitheliopathy, which increase at distinct stages of disease severity in COVID-19.”
Even in patients who are not critically ill, the higher levels of angiogenic factors may indicate the presence of low blood oxygen levels because of pulmonary injury, which means they require supplemental oxygen.
In those patients with a critical illness, there is a significant increase in these biomarkers, which indicates that endothelial damage is a significant contributor to thrombosis and multiple organ breakdown, these being signs of critical disease.
Implications and Future Directions
Earlier work has shown that markers like D-dimer, troponin, and B-type natriuretic peptide are associated with lower mortality in this condition. However, few studies report how vascular biomarkers can be used to predict survival in these patients. This is a significant knowledge gap since endothelial injury is being shown to be a key player in severe COVID-19.
Moreover, if circulating markers are developed that can pick up specific aspects of the disease process, they could help to roll out newer therapeutic tools. For instance, dipyridamole, a platelet aggregation inhibitor, and complement inhibitors could be used to protect the blood vessels against COVID-19 damage.
The researchers point forward, “Further validation of our findings in larger patient cohorts, together with mechanistic studies to understand the causes of endothelial injury and its consequences for immune activation, vascular dysfunction, and thrombosis, promise to provide pivotal insights into COVID-19 pathogenesis and guide clinical management.”

 This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources