The COVID-19 pandemic shows no signs of abating, with outbreaks in many spots still occurring across the world. From the start, health organizations and governments were focused on implementing non-pharmaceutical interventions (NPIs) in the absence of any effective antivirals or vaccines. Now, a new study published on the preprint server medRxiv* in August 2020 discusses how these NPIs helped to shape the course of the pandemic.
Mostly NPI strategies were shaped by looking back at what worked during the earlier outbreaks of H1N1 flu, severe acute respiratory syndrome (SARS), and Middle East Respiratory Syndrome (MERS) epidemics. Moreover, the Chinese lockdown implementation bolstered by mathematical models and observations on current trends helped to set up NPI approaches, though these varied by timeline, country, and severity.
Some of the common NPIs included school and workplace closures, social distancing, prohibiting or severely limiting public gatherings, the use of face masks outside one’s house, or when interacting with individuals outside one’s household, and shelter-in-place orders, neighborhood quarantines, and national lockdowns. All NPIs are designed to reduce the contact between infected and non-infected cases, and thus flatten the curve of new infections. The researchers estimate that about 55% of the world’s population will have experienced some form of isolation as of April end, 2020.
The Effects of NPIs
The measurement of the effects of NPI implementation in a region is challenging in that transmission statistics are always inaccurate. This is due to significant variations in the way testing actually covers a target population, changes in testing strategies at various points, test reporting delays, and differences in the incubation period. As a result, the infected population at a given time point is difficult to assess with accuracy.
The solution some groups have employed is dynamic mathematical modeling. Evidence from such models has concluded that viral spread and COVID-19 deaths are reduced effectively by quarantine. However, these models are based on data from SARS and MERS epidemics, with only limited information on the current pandemic at that time point.
Another study from the European Centre of Disease Prevention and Control (ECDC) shows that the NPIs were estimated by experts to have reduced population contacts by 70%. Other studies support this figure, estimating that viral spread dropped by over 80%, and COVID-19 mortality by 3.1 million in the 11 countries of the study.
In yet another preprint paper, researchers found that viral transmission was not affected by lockdowns or social distancing. Instead, the researchers identified a mixture of school closures, the use of face masks, and centralized quarantine as required to control the epidemic rather than full lockdown.
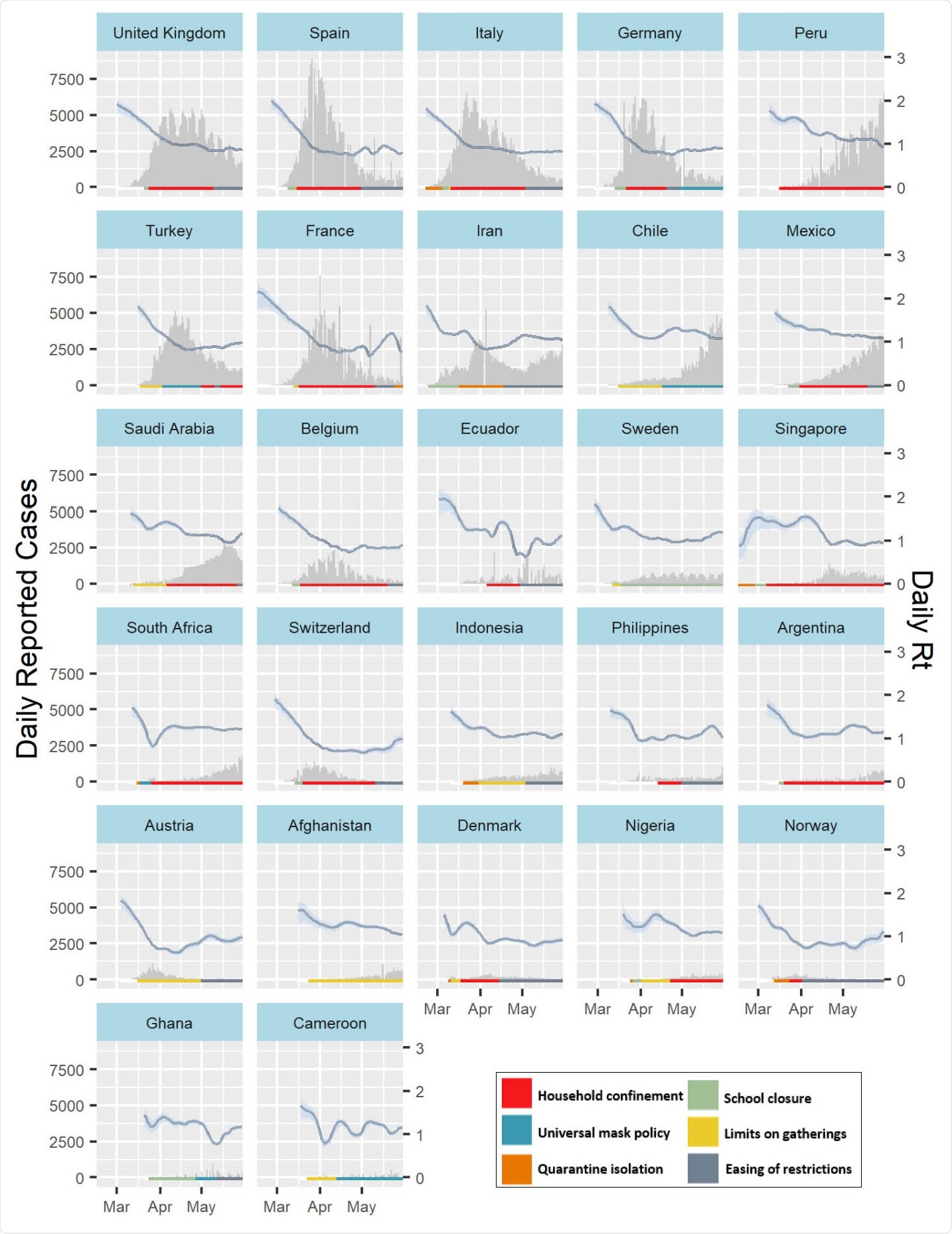
Timeline of daily reported COVID-19 incidence and implementation of non-pharmaceutical interventions across different countries (A) and US states (B). Plots are arranged by order of highest cumulative caseload as of May 31st, 2020, and illustrate the timeline of the implementation of quarantine and isolation policies (orange), limits on gatherings (yellow), school closures (green) and universal facemask policies (blue). We excluded other interventions implemented during time-periods of household confinement (red) and specified the date of easing of restrictions (grey) as defined in the methods. NPI timelines are illustrated alongside daily reported cases (grey bars) and the estimated daily Rt (blue line and ribbon representing median Rt and 0.05 – 0.95 quantiles respectively).
Analysis of Uncertainties
In the current study, the investigators used appropriate methods to capture the uncertainty in the reporting of data and the spread of the virus, to understand the impacts made by each of these measures over the course of the pandemic so far. This allowed them to take into account the later behavioral changes that followed the observation of the outbreak in the first few countries, such as China, South Korea, and several parts of Europe.
NPIs Follow Incidence Rates – Except in the US
The researchers considered only mandatory NPIs implemented over the whole nation (or state, in a federal set up). They finally had 145 events from 26 countries and 34 American states. They found that face masks and mandatory quarantine were often used along with other NPIs. Restrictions were being reduced in over 90% of countries in Europe, and over 70% of states in the US. However, African and South American countries still had several mandatory NPIs.
A striking observation was that unlike most other countries where the implementation or relaxation of such NPIs depended on the degree of control of the outbreak, the US had begun to ease restrictions even while the incidence was still going up in many places.
Earlier and More Drastic NPIs Have Greater Effects
Secondly, they observed that the higher the reproduction number Rt (the number of people to which one infected individual spreads the infection, on average), the higher was the drop in the relative change in Rt in response to the NPIs put in place earlier on in the pandemic’s course as opposed to later. The measures with the highest impact included lockdowns, limits on gatherings, school closures, and the wearing of face masks. These reduced the Rt by 23%, 10%, 12%, and 17%, respectively.
They also estimated both negative and positive impacts of relaxations where these had been carried out, as well as a 12% decline in the daily Rt over time when any measure was in place. The highest estimated fall in Rt was expectedly associated with stay-at-home policies.
The most significant drop in Rt was linked to the earlier implementation of NPIs, as reported by other modeling studies. However, they found it difficult to untangle the interlinked effects of the successive lifting of each NPI because, more often than not, such measures tend to be applied and lifted in groups.
The researchers operate under the hypothesis that all countries have experienced mass behavioral changes due to the pandemic, which deprives them of any counterfactual scenario to estimate the possible infection rates if no NPI was in place. The overall 12% fall in Rt with time was estimated to represent the impact of all the NPIs and changes in behavior, with a snowballing effect caused by increased global awareness. This makes this decline independent of the type of interventions or the sequence.
Timeline-Dependent Effect
The strong effect of complete lockdowns may be, in part, due to the lingering effect of prior interventions. The 23% reported drop with mandatory household confinement is far below the 81$ reported by other studies. The difference lies in the geographical and temporal variation in those countries since the previous study took place in 11 European countries, which were first affected and had mostly returned to normal by the time of the current study. In contrast, the current study included countries that are still reaching their infection peak, with smaller current drops in the Rt.
Timing Matters in Impact Size
Again, both the current and prior research shows that the current control in Wuhan, for instance, depended on the local restrictions on mobility before the complete lockdown was clamped down, and especially on the early implementation of these measures. Earlier studies have estimated that the number of cases could have gone up or down threefold if the NPIs had been put in place a week later or earlier.
The researchers have pointed out that daily confirmed case number is inaccurate in counting the infected population at any time point due to delayed reporting and inadequate testing. Secondly, without a sufficient gap between successive interventions, the impact of any given measure is lost in the overall impact of measures already in place, given the estimated 5-14 day incubation period.
Thus, the study confirms earlier research, showing that NPIs do reduce the rate of increase in case incidence globally, with earlier implementation being linked to more substantial impacts. This is still seen after adjusting for the time since the first 100 infections.
Implications and Future Directions
The inability to measure the impact of individual measures makes it difficult to predict whether such steps will help to achieve control of the outbreak in countries where the incidence is still going up. This should promote continuing research into the actual effectiveness and best combination of individual NPIs, using the data that is currently being gathered from all over the world. This will help with making decisions to handle the expected resurgence of the pandemic.

 *Important notice: medRxiv publishes preliminary scientific reports that are not peer-reviewed and, therefore, should not be regarded as conclusive, guide clinical practice/health-related behavior, or treated as established information.
*Important notice: medRxiv publishes preliminary scientific reports that are not peer-reviewed and, therefore, should not be regarded as conclusive, guide clinical practice/health-related behavior, or treated as established information.