The coronavirus disease 2019 (COVID-19), which is caused by the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), has caused damage and distress at an unprecedented scale worldwide. The respiratory pathology associated with COVID-19 is well established; however, there are also reports on the extrapulmonary manifestations of the disease which can include thrombotic complications, myocardial dysfunction, acute kidney injury, gastrointestinal symptoms, and neurological anomalies.
Earlier studies have identified neurological and psychiatric abnormalities in COVID-19 patients. An earlier report has identified molecular mimicry as a potential mechanism for the development of neuropsychiatric symptoms seen in COVID-19 patients.
The N-methyl-d-aspartic acid receptor (NMDAR) GluN1 and GluN2a subunits are structurally similar to the SARS-CoV-2 non-structural protein 8 (NSP8) and 9 (NSP9), respectively. This may result in molecular mimicry, wherein immunoglobulin G (IgG) antibodies elicited against the SARS-CoV-2 proteins NSP8 and NSP9 may cross-react with the host NMDAR and lead to the destruction of these receptors and subsequent neurological anomalies observed in COVID-19 patients.
Anti-NMDAR encephalitis is a commonly occurring autoimmune encephalitis and has been reported in viral infections such as herpes simplex 1 or varicella-zoster. The neurological manifestations of COVID-19 may be due to the secondary occurrence of anti-NMDAR encephalitis. In a recently published study in the Journal of Neuroinflammation, scientists explore the link between SARS-CoV-2 infection and anti-NMDAR encephalitis.
Key findings
The scientists in this study conducted a systematic review of literature in the PubMed and Google Scholar databases. The search terms they used include "NMDA encephalitis," "NMDAR encephalitis," "NMDA receptor encephalitis," and "SARS-CoV-2" or "COVID-19". They identified eight case reports of COVID-19 patients, aged between 23 months to 53 years, who developed anti-NMDAR encephalitis.
Of the eight patients identified, four were female and four male. The patients developed anti-NMDAR encephalitis three days to three weeks after the onset of COVID-19 symptoms. Notably, four of the patients developed encephalitis in less than one week.
All eight patients showed positivity for antibodies against NMDAR GluN1 subunit in the cerebrospinal fluid (CSF).
From the case reports identified, four of the patients showed symptoms of severe respiratory distress. All eight patients exhibited neuropsychiatric symptoms like disturbed consciousness, delirium, and psychosis, whereas six of the patients had suffered from epileptic seizures. Motor failures or dysarthria were observed in five patients.
The inflammatory marker interleukin-6 (IL-6) levels were found to be elevated in two patients. IL-6 levels were increased in both the blood and cerebrospinal fluid (CSF) of one patient and in the CSF alone of the other.
Elevated C-reactive protein (CRP) levels were observed in the blood samples of two patients. Decreased lymphocyte levels were observed in the blood samples of three patients. Interestingly, increased lymphocyte levels were observed in the CSF of six patients, including the ones who showed decreased lymphocyte levels in blood samples. Further, the CSF of two patients exhibited positivity for SARS-CoV-2.
Notably, one patient had an associated condition of ovarian teratoma, which is a contributing factor for anti-NMDAR encephalitis.
Electroencephalogram (EEG) recordings of four patients showed slow-wave activity, thereby implying brain abnormalities. One of these patients presented with an extreme delta brush-like pattern which is indicative of anti-NMDA receptor encephalitis. The case report of five patients showed normal brain images.
Fluid-attenuated inversion recovery (FLAIR) images of one patient showed hyperintensities in the left amygdala and left anterior putamen, with a mild effect in the right amygdala. This patient was initially negative for SARS-CoV-2 and later tested positive, thus suggesting the possibility of hospital-acquired infection.
The patients were treated based on standard guidelines and all of them were given steroid therapy along with intravenous IgG. Two of the patients also received plasmapheresis. The case reports of all eight patients showed that they improved after therapy.
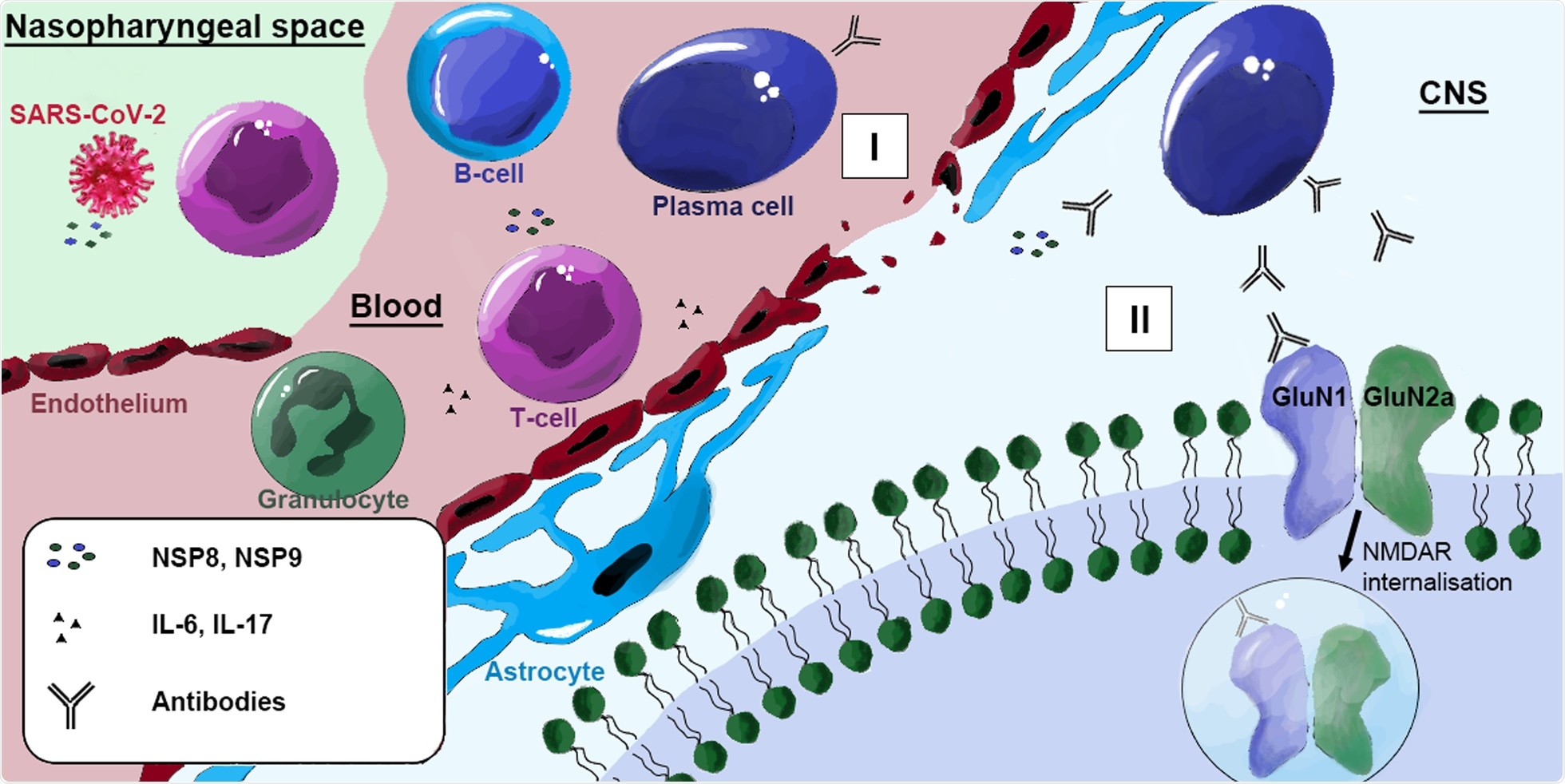 Possible pathophysiology of anti-NMDAR encephalitis induced by SARS-CoV-2. During acute COVID-19 infection, viral particles, including NSP8 and NSP9, are released. The released proteins are recognized by T cells, leading to activation of B cells, which become plasma cells and produce IgM and later IgG antibodies against NSP8 and NSP9. I SARS-CoV-2-associated endothelitis and IL-17 produced by activated T cells disrupt the blood-brain barrier, allowing NMDAR antibodies to enter the CNS. IL-6 alters glial activity and initiates neutrophil granulocyte migration leading to further blood-brain barrier destruction and inflammation. II Due to molecular mimicry, antibodies produced by plasma cells in the CNS can cross-react with the NMDAR subunits GluN1, leading to receptor internalization with subsequent degradation.
Possible pathophysiology of anti-NMDAR encephalitis induced by SARS-CoV-2. During acute COVID-19 infection, viral particles, including NSP8 and NSP9, are released. The released proteins are recognized by T cells, leading to activation of B cells, which become plasma cells and produce IgM and later IgG antibodies against NSP8 and NSP9. I SARS-CoV-2-associated endothelitis and IL-17 produced by activated T cells disrupt the blood-brain barrier, allowing NMDAR antibodies to enter the CNS. IL-6 alters glial activity and initiates neutrophil granulocyte migration leading to further blood-brain barrier destruction and inflammation. II Due to molecular mimicry, antibodies produced by plasma cells in the CNS can cross-react with the NMDAR subunits GluN1, leading to receptor internalization with subsequent degradation.
How does anti-NMDAR encephalitis develop in SARS-CoV-2 infection?
Anti-NMDAR encephalitis, caused by IgG antibodies acting against the GluN1 subunit of NMDAR, is a commonly occurring form of autoimmune encephalitis.
Upon infection with SARS‐CoV‐2, viral particles such as NSP8 and NSP9 are released. These proteins, when recognized by T-cells, result in the activation and transformation of B-cells into plasma cells. This results in the production of IgM and IgG antibodies by these plasma cells, which act against NSP8 and NSP9.
The blood-brain barrier (BBB) may be destroyed in COVID-19 patients due to several contributing factors including IL-17 produced by activated T-cells, SARS-CoV-2 associated endothelitis, which is inflammation of blood vessels, and neutrophil granulocyte migration caused by IL-6 mediated alteration of glial activity. The damage to the BBB may lead to the entry of these antibodies into the central nervous system (CNS), which may cross-react with the NMDAR subunit GluN1. This may result in internalization and degradation of the NMDAR, thus disrupting the excitatory glutamatergic transmission causing anti-NMDAR encephalitis.
Further investigations are required to arrive at conclusive evidence about the mechanism through which SARS-CoV-2 infection results in the secondary occurrence of anti-NMDAR encephalitis.
Limitations
The scientists only identified eight case reports of patients with SARS-CoV-2-related autoimmune anti-NMDAR encephalitis, which is a small number that limits the possibility of conclusive evidence. In one of the patients' manifestations of anti-NMDAR encephalitis, symptoms preceded SARS-CoV-2 test positivity, whereas another patient had a pre-existing ovarian teratoma which is also a contributing factor for anti-NMDAR encephalitis.
In the case reports of these two patients, a definitive association between SARS-CoV-2 infection and the subsequent development of anti-NMDAR encephalitis cannot be established. Further investigations are required to confirm the role of SARS-CoV-2 in the development of anti-NMDAR encephalitis in COVID-19 patients.
Conclusions
Secondary occurrence of anti-NMDAR encephalitis with neuropsychiatric symptoms following COVID-19 has been demonstrated in this systematic review for the first time. Though the investigations in this review are preliminary, these findings highlight the importance of considering the presence of neurological anomalies while treating COVID-19 patients.
The findings presented here suggest a need to monitor COVID-19 patients for neurological symptoms of autoimmune encephalitis such as seizures, psychotic symptoms, headache, dizziness, dyskinesias, memory changes, and catatonia. It is also important to screen COVID-19 patients for neurological abnormalities using brain imaging, EEG recordings along with cell-based assays for detecting the presence of anti-neuronal antibodies employing serological and CSF tests. Early immunotherapy for COVID-19 patients diagnosed with autoimmune encephalitis may be an effective treatment strategy based on the observations from this review.
Journal reference:
- Vasilevska, V., Guest, P. C., Bernstein, H., et al. (2021). Molecular mimicry of NMDA receptors may contribute to neuropsychiatric symptoms in severe COVID-19 cases. Journal of Neuroinflammation 18(245). doi:10/1186/s12974-021-02293-x.