Introduction
The resurgence of measles
The role of vaccine hesitancy
Consequences beyond infection
Counteracting the crisis
Looking ahead
References
Amid a dramatic rise in measles cases globally, vaccine hesitancy and misinformation are undermining decades of progress, putting vulnerable populations and health systems at risk. Discover the causes, consequences, and solutions to this preventable public health crisis.
 Image Credit: Tarwar65 / Shutterstock.com
Image Credit: Tarwar65 / Shutterstock.com
Introduction
Measles is a highly contagious disease caused by a virus belonging to the genus Morbillivirus that rapidly spreads through respiratory droplets. Measles symptoms include a characteristic red rash, as well as cough, high fever, inflamed eyes, and runny nose.1,2 Infants and young children under five years of age are most susceptible to this infection, particularly those who are unvaccinated or immunocompromised.3,4
A safe and effective measles vaccine has been available since 1963, with comprehensive vaccination efforts nearly eradicating measles in the U.S. In regions with low vaccination coverage, measles remains a global health threat that is responsible for substantial mortality, primarily among unvaccinated children.4,5
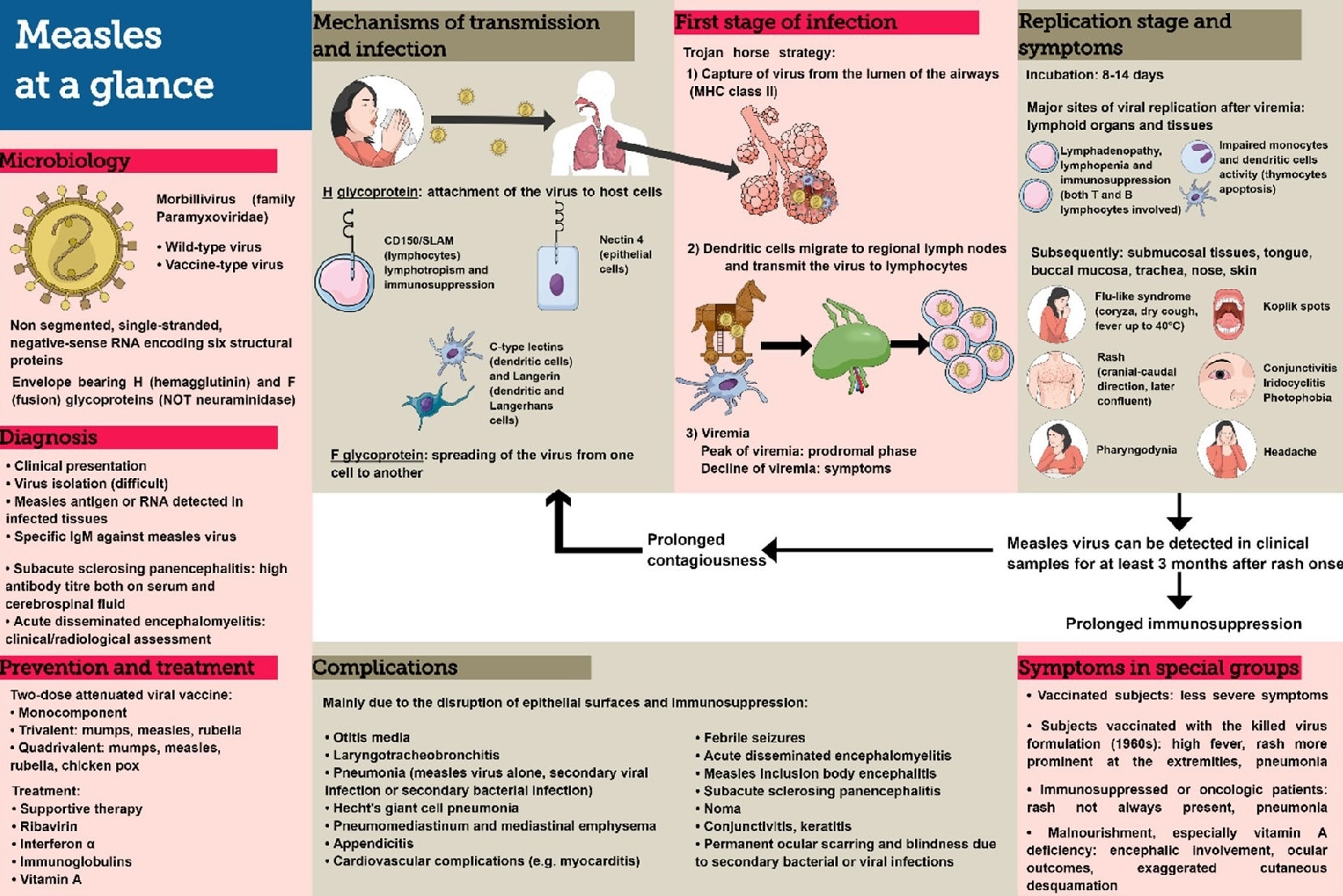 ”Measles at a glance”: microbiology, mechanisms of transmission and infection, symptoms, complications, diagnosis, prevention and treatment.2
”Measles at a glance”: microbiology, mechanisms of transmission and infection, symptoms, complications, diagnosis, prevention and treatment.2
The resurgence of measles
In 2024, the European Union/European Economic Area (EU/EEA) recorded over 35,000 measles cases, a ten-fold increase from the previous year. About 87% of known measles cases were reported in unvaccinated individuals.1
As of March 2025, over 220 cases of measles have been confirmed across multiple states in the U.S., with children five years of age and younger accounting for over one-third of infections.6
Hospitalizations have been common, and fatalities, though still rare, have occurred. In Romania alone, 22 of 23 measles deaths in 2024 occurred in children under five.1
Complications such as pneumonia, encephalitis, and subacute sclerosing panencephalitis (SSPE) are also serious risks associated with measles infection, particularly for young children and immunocompromised individuals.3
Measles is currently spreading in clusters, often within tight-knit or under-immunized communities. In the U.S., outbreaks have emerged in states such as Texas, New York, and California, all of which are regions with both high population density and notable vaccine exemption rates.5
Romania also serves as a hotspot for measles cases, as this country accounts for nearly 87% of EU/EEA cases in 2024.1 Similar trends have been observed in other high- and middle-income nations, where vaccine coverage has declined below the 95% threshold needed to maintain herd immunity.7
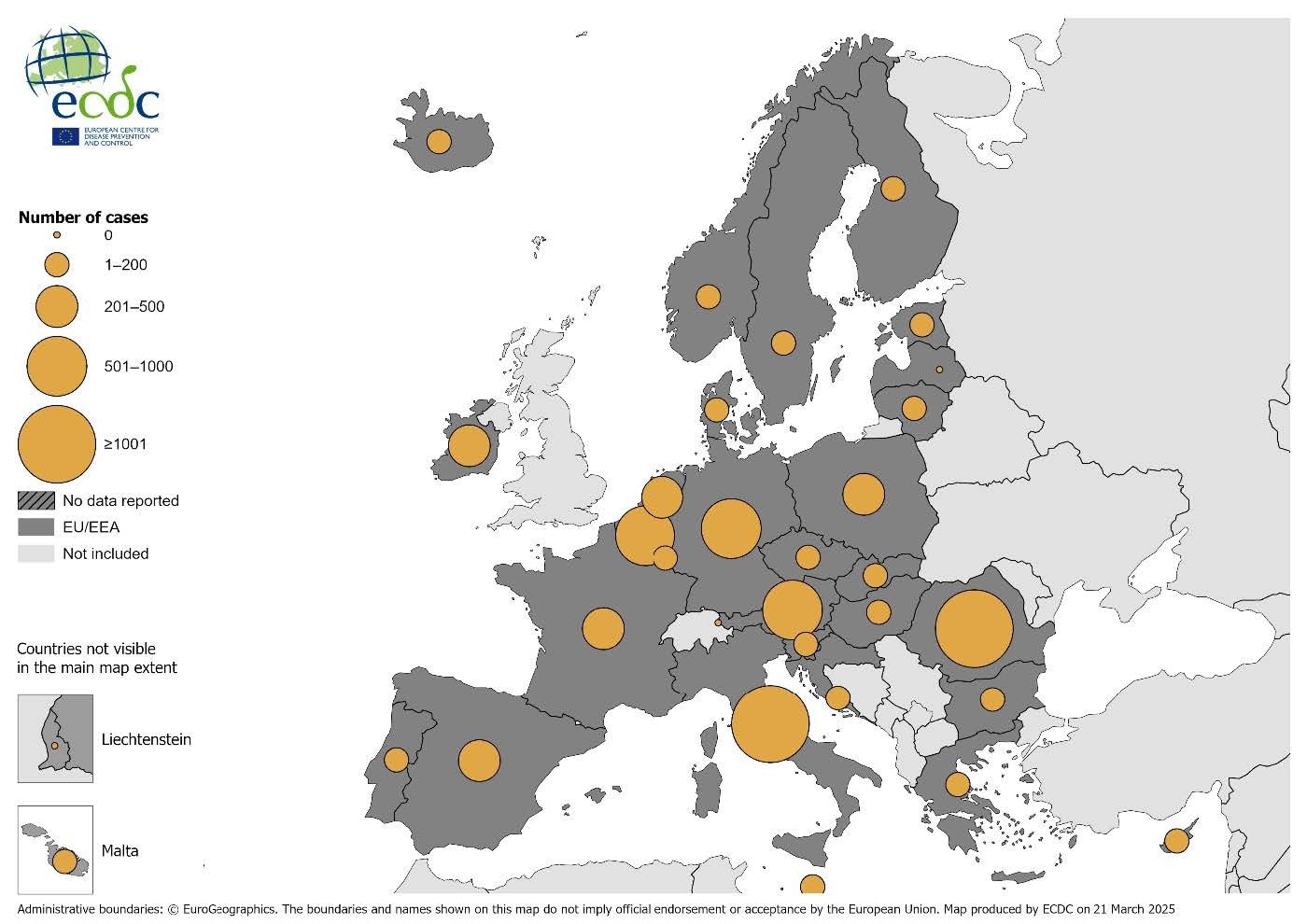
Number of measles cases by country, EU/EEA, 2024. Source: Country reports from Austria, Belgium, Bulgaria, Croatia, Cyprus, Denmark, Finland, France, Germany, Greece, Hungary, Iceland, Ireland, Italy, Latvia, Liechtenstein, Lithuania, Luxembourg, Malta, the Netherlands, Norway, Poland, Portugal, Romania, Slovakia, Slovenia, Spain, Sweden.
The role of vaccine hesitancy
The resurgence of measles is not a failure of science but of communication, trust, and policy. Vaccine hesitancy, which is the refusal or delayed acceptance of vaccines despite availability, has emerged as a key driver of the re-emergence of measles.
Misinformation about vaccine safety, particularly false claims linking the measles, mumps, and rubella (MMR) combined vaccine to autism, has fueled public fear and skepticism.4 Social media platforms have amplified anti-vaccine narratives, often more rapidly than public health agencies can counter them. The result is a decline in vaccine confidence, especially among parents making decisions for young children.6
Growing distrust in the government and medical institutions, compounded by the politicization of public health during the COVID-19 pandemic, has eroded vaccine uptake.8 Religious and philosophical exemptions from vaccination have similarly contributed to under-immunized clusters, thus facilitating measles outbreaks in regions where overall vaccine availability is not the limiting factor.5,9
Dr. Adam Ratner, director of the Division of Pediatric Infectious Diseases at New York University (NYU) Langone Health, states that even though measles is one of the most contagious human diseases, it is entirely preventable with the vaccine, but it can be fatal for partially vaccinated or unvaccinated populations, especially children.10
Measles outbreak spreads to 15 states with cases on the rise
Consequences beyond infection
Each measles outbreak places a substantial burden on the financial and operational infrastructure of healthcare systems. Containing a single measles outbreak can require thousands of staff hours for contact tracing, emergency immunizations, and public health messaging.8 Hospitalizations, isolation protocols, and complications such as encephalitis or pneumonia also increase strain on public health budgets and resources.8
Responding to measles outbreaks imposes a significant economic burden on public health systems. Each measles case can cost public agencies between $48,000 and $142,000 in direct response efforts such as case investigation, laboratory testing, contact tracing, post-exposure prophylaxis, and emergency vaccination campaigns.11
These costs scale rapidly during large outbreaks. For example, the 2019 New York outbreak exceeded $8.4 million in public health response expenditures.
Localized outbreaks divert funding and staffing from other essential services, thus weakening the resilience of public health infrastructure. In fact, recent studies have confirmed that measles outbreak costs significantly exceed the cost of prevention through routine immunization programs.5,9
The resurgence of measles also endangers the health of infants who are too young to be vaccinated, immunocompromised individuals, and pregnant women, all of whom are particularly vulnerable to severe outcomes.2
Counteracting the crisis
In response to the resurgence of measles, public health institutions have implemented a wide range of strategic interventions to increase vaccination rates, rebuild public trust, and address systemic barriers to immunization.
One of the primary approaches has been the rollout of large-scale vaccination campaigns and, in some areas, the declaration of public health emergencies to mobilize resources and ensure that unvaccinated populations are identified and vaccinated promptly.1
Policy changes have also been implemented, with several governments eliminating non-medical exemptions for school entry, thereby reducing the number of children attending educational institutions without immunization. For example, following a significant outbreak linked to Disneyland, California lawmakers passed legislation that led to a substantial increase in MMR vaccine coverage statewide.5
Health professionals and community advocates must also engage with and educate communities to dispel myths and misinformation surrounding vaccine safety. Interactive campaigns that include workshops, social media engagement, and school-based initiatives have shown promise in reversing hesitancy, particularly when they are specific to the values and concerns of each community.8
In many settings, these engagement strategies have shifted public perception and increased willingness to vaccinate. However, the long-term success of these programs depends on sustained investment, government efforts, and public cooperation to ensure comprehensive and consistent vaccination coverage.
Looking ahead
To regain control over measles and other vaccine-preventable diseases, a comprehensive and multi-factorial approach is essential. Rebuilding public trust in medical institutions remains a top priority and requires transparent, empathetic, and consistent communication. Educational initiatives must address vaccine safety and the severe consequences of preventable diseases, with messaging tailored to the cultural and regional needs of specific communities.4
Technological innovations such as microarray patches (MAPs) also offer promising solutions to improve vaccine accessibility and acceptance by removing barriers associated with needle-based delivery systems and streamlining distribution logistics.8
Given the high transmissibility of measles, effective control depends on strong global coordination to enhance disease surveillance, maintain robust routine immunization programs, and ensure rapid outbreak response across both high- and low-resource regions.7
References
- European Centre for Disease Prevention and Control. Measles. In: ECDC. Annual Epidemiological Report for 2024. Stockholm: ECDC; 2025, https://www.ecdc.europa.eu/en/publications-data/measles-annual-epidemiological-report-2024
- Misin, A., Antonello, R. M., Di Bella, S., Campisciano, G., Zanotta, N., Giacobbe, D. R., Comar, M., & Luzzati, R. (2020). Measles: An Overview of a Re-Emerging Disease in Children and Immunocompromised Patients. Microorganisms, 8(2), 276. DOI:10.3390/microorganisms8020276, https://www.mdpi.com/2076-2607/8/2/276
- Gastanaduy, P. A., Funk, S., Lopman, B. A., Rota, P. A., Gambhir, M., Grenfell, B., & Paul, P. (2020). Factors Associated With Measles Transmission in the United States During the Postelimination Era. JAMA Pediatrics, 174(1), 56–62. DOI:10.1001/jamapediatrics.2019.4357, https://jamanetwork.com/journals/jamapediatrics/fullarticle/2755836
- Parums D. V. (2024). A Review of the Resurgence of Measles, a Vaccine-Preventable Disease, as Current Concerns Contrast with Past Hopes for Measles Elimination. Medical Science Monitor, 30, e944436. DOI:10.12659/MSM.944436, https://medscimonit.com/abstract/full/idArt/944436
- Feemster, K. A., & Szipszky, C. (2020). Resurgence of measles in the United States: how did we get here?. Current Opinion in Pediatrics, 32(1), 139–144. DOI:10.1097/MOP.0000000000000845, https://journals.lww.com/co-pediatrics/abstract/2020/02000/resurgence_of_measles_in_the_united_states__how.19.aspx
- Weiss, A., & Ding, Y. (2025). The resurgence of measles in the US: A consequence of vaccine hesitancy and spread of misinformation. Environmental Disease, 10(1), 1–3. DOI:10.4103/ed.ed_2_25, https://journals.lww.com/endi/fulltext/2025/01000/the_resurgence_of_measles_in_the_us__a_consequence.1.aspx
- Bidari, S., & Yang, W. (2024). Global resurgence of measles in the vaccination era and influencing factors. International Journal of Infectious Diseases, 147, 107189. DOI:10.1016/j.ijid.2024.107189, https://www.sciencedirect.com/science/article/pii/S1201971224002601
- Pasadyn, F., Mamo, N., & Caplan, A. (2025). Battling measles: Shifting strategies to meet emerging challenges and inequities. Ethics, Medicine and Public Health, 33, 101047. DOI:10.1016/j.jemep.2025.101047, https://www.sciencedirect.com/science/article/pii/S2352552525000064
- Dimala, C. A., Kadia, B. M., Nji, M. A. M., & Bechem, N. N. (2021). Factors associated with measles resurgence in the United States in the post-elimination era. Scientific Reports, 11(1), 51. DOI:10.1038/s41598-020-80214-3, https://www.nature.com/articles/s41598-020-80214-3
- The University of Chicago. (2025, February 20). Podcast: Why measles is resurging—and the rise of vaccine hesitancy, with Adam Ratner. University of Chicago News. https://news.uchicago.edu/big-brains-podcast-why-measles-resurging-and-rise-vaccine-hesitancy
- Pike, J., Melnick, A., Gastañaduy, P. A., Kay, M., Harbison, J., Leidner, A. J., Rice, S., Asato, K., Schwartz, L., & DeBolt, C. (2021). Societal Costs of a Measles Outbreak. Pediatrics, 147(4), e2020027037. DOI:10.1542/peds.2020-027037, https://publications.aap.org/pediatrics/article-abstract/147/4/e2020027037/180774/Societal-Costs-of-a-Measles-Outbreak?redirectedFrom=fulltext
Last Updated: May 18, 2025