Skip to:
What is Arthritis?
Arthritis, derived from Greek for “disease of the joints,” is the chronic or acute inflammation of joints, which is often accompanied by structural damage and pain. In contrast, rheumatism is an informal term used to describe joint diseases or syndromes.

Image Credit: Anut21ng Photo / Shutterstock
Medical literature does not generally use the term rheumatism. Instead, arthritis is commonly used to refer to such conditions.
Arthritis is characterized by joint abnormalities, stiffness, and pain caused by inflammation. Inflammation can be caused by several factors including:
- Infections such as those seen in septic arthritis
- Auto-inflammatory or auto-immune mechanisms are seen in rheumatoid arthritis
- Crystal deposits such as gout
- Degenerative diseases such as osteoarthritis
- Inflammation can sometimes be idiopathic, i.e., arise with no specific cause
Similarly, many individuals can subsequently develop arthritis following the onset of another disease, for example, Lyme disease, celiac disease, lupus, and psoriasis.
The condition is considered to affect more than 10 million people in the UK from all age groups, including children. There are multiple types of arthritis with rheumatoid arthritis and osteoarthritis being the most prevalent types.
Due to the different types, symptoms experienced tend to vary. However, common symptoms include:
- Muscle weakness and wasting
- Limited mobility of the joints
- Joint stiffness, pain, and sensitivity
- Inflammation of the joint and surrounding areas
- Warm skin covering the affected joint
Rheumatoid Arthritis
Rheumatoid arthritis (RA) commonly affects those aged between 40 and 50 years old and is three times more prevalent in women than men.
RA develops in response to the body’s immune system attacking specific joints leading to an inflammatory response and pain. During this process, the synovium, the outer covering of the joint, is first affected.
Damage can then spread to other areas of the joint, causing increased swelling and altering the joint’s overall shape and structure. This can adversely impact the cartilage and bone by causing it to break down.
Osteoarthritis
Osteoarthritis typically affects those aged 40 years old or older, women, and those with a family history of the condition. However, it has been found to develop at any age due to injury or other comorbid joint conditions such as rheumatoid arthritis.
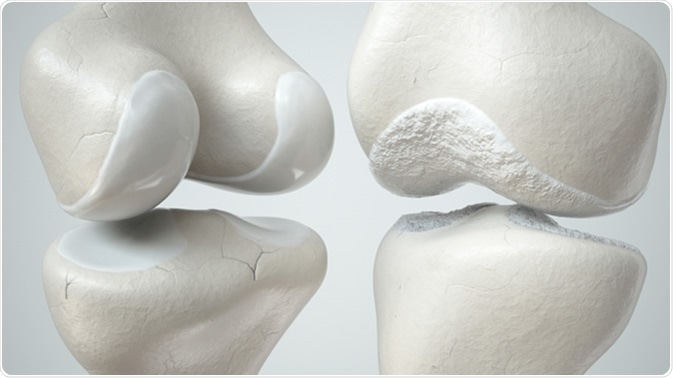
Healthy and osteoarthritis-covered knee - 3D render. Crevis / Shutterstock
Osteoarthritis affects the smooth cartilage that lines the joint and leads to reduced mobility, stiffness, and pain. Swelling and osteophytes can develop as a result of ligaments and tendons having to work harder to compensate for the thinning cartilage lining.
How is Arthritis Diagnosed?
Imaging technology is often used by physicians to diagnose arthritis as well as to measure the severity of the condition.
The underlying pathology, the level of joint destruction, and the integrity and stability of nearby structures can be determined using MRI, ultrasound, CT, and X-rays. For those with arthritis that affects the hand, bone scanning is often used to show the symmetrical joint involvement.
Further tests include analyzing the patient’s joint fluid to examine their white and red blood cell counts, amongst other factors. This can be useful in ruling out an inflamed or septic joint.
Treatment of Arthritis
Arthritis is considered a progressive condition with no cure. Patients whose condition progresses rapidly tend to be older, have multiple affected joints, or are obese. There are some treatment options for those with RA and osteoarthritis.
Treatment for Rheumatoid Arthritis
Typically, those with RA will be prescribed disease-modifying anti-rheumatic drugs (DMARDs). DMARDs help to relieve the symptoms experienced and reduce the rate of progression.
The medication improves symptoms by limiting the effects of the chemicals synthesized as a result of your immune system, attacking the joints.
Other treatments include biological treatments, for example, infliximab and etanercept, which are typically taken alongside DMARDs.
Usually, taken by injection, the drug helps to prevent chemicals present in the blood from signaling to your immune system to attack the joints. Steroids may also be prescribed to help address the inflammation, pain, and stiffness.
Treatment for Osteoarthritis
For those with mild symptoms of osteoarthritis, several lifestyle changes are recommended to help manage symptoms. These include:
- If overweight, losing weight
- Wearing appropriate footwear
- Exercising regularly
- Using devices that help to reduce the amount of strain placed on the joints daily
In cases of more severe symptoms, pain killers may be prescribed in addition to an exercise plan to be followed with a physiotherapist.
Surgery may be recommended for a small proportion of patients where previous treatments have been deemed ineffective.
The surgery aims to replace any severely damaged joints or to repair or strengthen affected joints.
Rheumatic Diseases: Mayo Clinic Radio
Further Reading
Last Updated: Feb 17, 2023