The retina is part of the structure at the back of the eye and it is one of the three key layers of the tissue of the eye. You have the sclera, choroid and then you have the inner layer called the retina.
The critical part of the retina is found at the back of the eye in the centre, located very close to the optic nerve, this region is called the macula.
Within the macula, there's an area called the fovea, which is a little dip. The retina is made up of multiple layers, in the most inner layer at the back of the retina you find the photoreceptors, which are the key cells responsible for converting light into electrical signals - the first key step of the formation of vision.
The eye itself is often compared to a camera with a lens, shutter, and an aperture. With the retina at the back converting light into electrical signals and processing visual information, I would say it is the most complex biological computer.
The retina and the optic nerve are the outgrowth of the developing brain and it is considered to be part of the central nervous system - actually brain tissue. There are two main kinds of photoreceptors, rods and cones. There are 120 million rod cells in the retina and roughly 6 million cone cells, 2.5-3 million ganglion cells, and they have varying degree of concentration. In the central foveal part, you find the majority of the cones. In the outer para-foveal part of the retina, in your peripheral vision, you find mainly the rods.
Vision is formed in the brain, not in the eye. The eye is simply a processor of the visual part of the information, but the brain receives information from all your other senses to form a vision.
Imagine that you're standing in a corner and you hear a motor bike coming from somewhere, but you haven't seen it yet, your brain is already guessing that it is going to be a motor bike. If a horse then came around the corner, your brain would be very surprised.
Vision is done in your brain based on associative information that you learn over time, based on the updated information which comes from your eyes, but also relying on sound, touch, smell, balance, and hearing. All this is part of the vision formation.
What causes the degeneration of photoreceptors?
There are two primary reasons for degeneration of the functioning of the photoreceptors.
The first main reason is genetic, there are over 60 genes which can affect the photoreceptors, and there are over 200 mutations that lead to the degeneration of these in people suffering Retinitis Pigmentosa.
Retinitis pigmentosa starts typically with the rods in the outer part of the retina, and then slowly progressing, you find these people experiencing tunnel vision, as these cells start dying, because of the malformation. The rods die first and then slowly, it is like seeing the world through a straw. You still have some cones left in the middle and then over time the cones also die and the photo receptor layer is no longer functioning.
The second reason is more mechanistic due to age. The lipids, which are cleaning and replacing the functioning photoreceptors, are no longer very effective. These lipids that collect as a thick layer at the photoreceptor level, and starts blocking the cleaning up of the photoreceptors are called Drusen. Typically, that happens more in the central foveal region, and so effecting the cones more, which then start dying in the middle and it is more the central vision for the aged population that is affected, and they see little dark spots in the middle of their vision, so they cannot recognize faces or read.

How have advances in neurobiology, visual processing, microelectronics/nanoelectronics, optoelectronics, and intelligent software algorithms made bionic vision restoration technologies a possibility?
The advancement of technologies in the labs has allowed researchers to see what is going on with the biology at the cellular level and people began to understand that even if the photoreceptors have died, the rest of the visual pathway was still open.
How could you bypass that first step of light conversion into electrical signals? The retinal surface at back of the eye is very accessible, as the retinal tissue is the extension of the brain tissue and can be accessed via the ganglion cells forming the beginning of the optic nerve.
By stimulating the retinal surface, as the signals are coming in at the ganglion cell layer, which is the entry to the optic nerve, people described that they could see flashes of light.
The principle was known, but the technology was not there 20 years ago. Researchers believed that if you could do that chronically, you could re-establish light back into the brain.
The company Pixium Vision, figured out that you could build microelectronics to place permanently in the eye and get the signal back to the eye. By short cutting the biological pathway, which is coming from the non-functional photoreceptors, they can directly stimulate the surface of the retina, which are the retinal ganglion cells, and the person will be able to perceive something.

Experiments were completed over 15 years ago, and the challenge was that the technology was not yet stable and not yet miniaturized enough to replace permanently. For example, the challenge from an engineering point of view was, imagine you have a television, you want to place it in the Mediterranean Sea, which is also warm, moving and very salty. The environment in your eye is also salty water and warm and it is moving. You've got to put microelectronics in that environment.
Hermeticity, the encapsulation of electronics, is vital as you cannot let electronics to be exposed to salt water, which brings challenge of material corrosion.
You can do this acutely by poking the back of the eye with micro electrodes, but how do you put something there that will stay there and remain functioning? What you're asking to do is put the TV in the Mediterranean Sea and expect it to work, and a possibility to replace if it stops or if a better model of the TV comes along.
The challenge was to build something, that will stay there and will stimulate the beginning of the optic nerve allowing the person to perceive these light signals coming back into the brain. There were also parallel developments going on with optoelectronics, microelectronics, miniaturization, MRI imaging, and signal processing. The advances and problem solving from Pixium, was contributing towards research into putting this miniaturized and encapsulated form of electronics in the back of the eye to establish a signal, start stimulating and re-establish the signal processing to the brain, and a way to exchange the implant if needed.
The understanding of the mechanism of how the retinal signals work, combined with the advances in all these technological and scientific areas led to the Pixium's mission to convert light into vision. Converting light back into form of vision, which is technically converting photons in a specific way into signals that the neurons in your brain will understand. Expertise from multiple disciplines had to come together.

How important is Pixium Vision’s collaboration with academic and research partners such as the Institut de la Vision in Paris, the Hansen Experimental Physics Laboratory at Stanford University, and Moorfields Eye Hospital in London?
Pixium Vision is primarily a group of scientists and biomedical engineers, who create hardware and software algorithms and put active biocompatible material in the body. There is a third component in the world of systems, which is what I call the ‘wet ware’, which is the brain. You need to actually teach the brain something new.
Obviously, it would be impossible to have all this specialist knowledge within Pixium and so we are part of an ecosystem of global partners at the cutting edge of neuroscience, microsurgery, ophthalmic surgery, physics, optics and mathematics, because you are building surgical implant and hardware, software, and wet ware, which involves retraining the brain.
The brain is very plastic, which means that the brain is able to adapt to new signals. In the case of bionic vision restoration, the photoreceptors have died, the brain is not receiving anything biologically, and you are going to then send something which is artificial, prosthetic, and has been created outside the body.
Pixium relies on this ecosystem of partner research labs like the Hansen Physics Lab from University of Stanford. It relies on the hospitals for retinal surgery expertise like the Rothschild Hospital in Paris, or Moorfields Eye Hospital in London who have the expertise in the microsurgery needed for putting the implant in the eye and then you have the Vision Institute here in Paris who conducted research to understand the mechanisms of how the retina processes information.
Since the visual signal is not going to be following completely the natural pathway, something we must consider is the kind of signal we need to be sending so that the brain will accept it. To give you an example, if you do not speak Chinese and you are standing in front of Chinese symbols and there is nobody there to explain them to you, it will be difficult for you to know what all those symbols mean if you've never seen them before. Artificial vision or bionic vision is like that.
We are very dependent on these academic and research experts to help us build the surgical technique to place these things in there and build the system and training required afterwards to be sending information that the brain will understand. You are teaching the brain of those who are blind and have no longer any external reference, but they have the history of vision that you are trying to bridge.
That's why we don't work at the beginning with people who are born blind, because we want to be able to communicate. These experts around us in our network of consultants and partners who help us develop the whole system are critical to the success on this journey, which was not so long ago considered impossible.
Giving sight back to the blind was considered either a biblical miracle or science fiction. It has now, however, become possible, scientifically. I would say it is a scientific miracle as a result of the ecosystem of experts, and the advances in technology being brought together and concentrated to solve this epic challenge.
Do you think it will be possible to replicate the physiological functions of the eye's photoreceptors and restore sight?
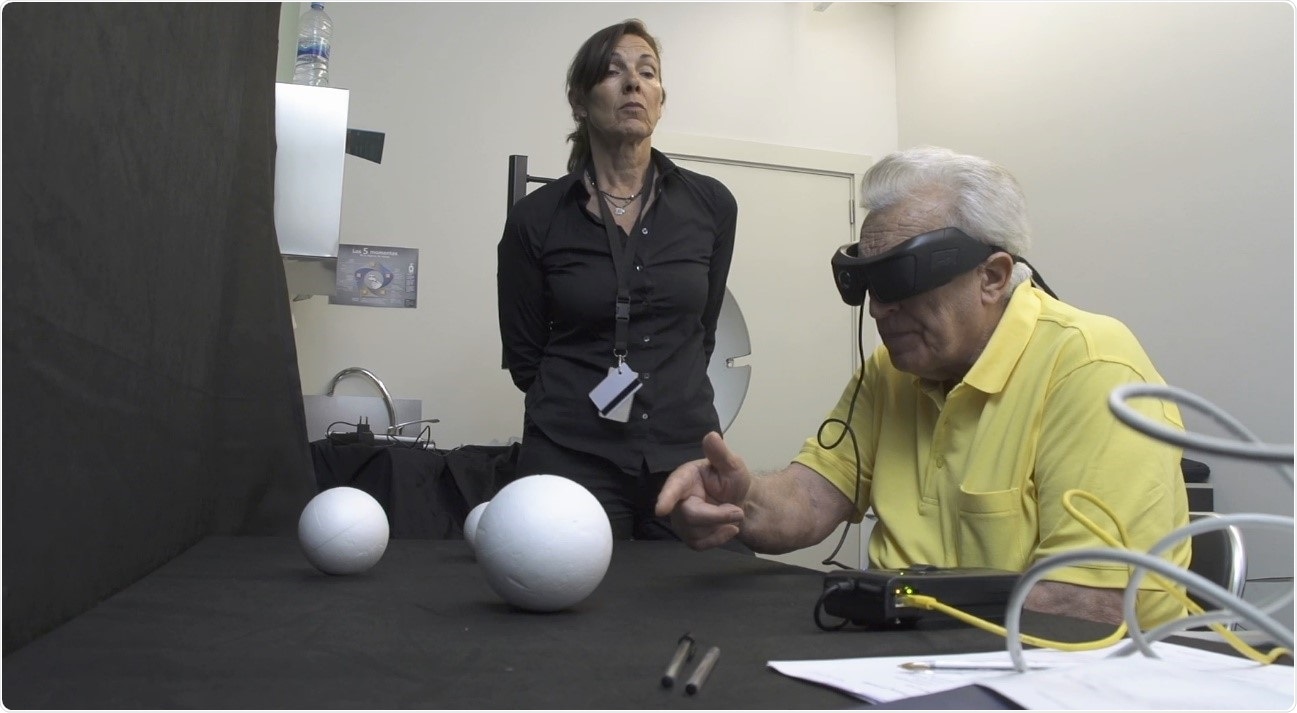
People are already able to have a useful visual perception. I will not call it vision at this point, because it is not natural vision, they start to re-establish useful patterns of these lights. Today, the objective of the first generation of these devices was to enable these people to perceive something which allows them to orient themselves to be more independent and to live more independent lives.
This may not sound like a lot, but for somebody who was in the darkness, having even this little useful perception back is a lot to them. This allows them to be more independent and to execute some tasks, some patients were able to see shapes, be able to tell whether the stairs are going up or down in front of them, see an outline of a person or an object, grasp an object on a table without spilling a glass of water, etc. Those are interactions which mean a lot in social interactions because being blind and in darkness is quite a challenge for them.
I would say today we are at a stage where it is a useful form, it is a partial restoration, we are bringing them from darkness into low vision status, which is a situation they may remember, because we are treating progressive diseases of blindness. They had vision at one point and progressively they were losing it, so they are classified as low vision to ultra-low vision at some point, then entering darkness. We're coming from darkness into low vision and then they have to learn how to use this visual perception in daily life for useful purposes. That's where we are today.

What are the main challenges that need to be overcome?
At this point, we are still at an insufficient level for people, because once you had something, people obviously want to get back to what they had before. That's the main expectation from the point of view of the blind themselves.
From the healthcare professionals, for them the argument is a little more technical, they're hoping we can get them back to at least to be able to read large letters in a low vision kind of stage, which they are used to, and can we get them to recognize faces again. Those are the kinds challenges that are next for us on this journey.
I often compare it to coming from the aeronautic space, and the space program where we are the first astronauts who are at the edge of space and they have come back and they are telling us what they experienced, perceived, and how they felt.
Unfortunately, we are not inside their brains, and so we are dependent on how they describe what they are perceiving at this point and the challenge from a biomedical engineering point of view. How can we then further improve the processing and replicate the functioning of the human retina to have the brain perceive something more detailed? Face recognition and reading a book again is to me the ultimate goal and we must get to it in steps.
Right now, the first patients are telling us that they can see shapes and objects and that they can orient and navigate better. The next goal for them is clearly to be able to read large letters, to be able to see clearly multiple objects in the environment around them, to navigate without falling down and the Holy Grail as a next step, is to get closer to face recognition and reading.
The closest proxy was the cochlear implants for sensory loss, people who have gone deaf. A similar approach was used to create artificial sound, 20 years ago and this was a field I spent some time in during 2001-2003. Early on, the bionic sound that people heard was very metallic, like a computerized voice, which is unpleasant to listen to over a long time.
Since then the algorithms, mathematics and signal processing has become very intelligent and now we're used to, in consumer products, wearing headphones that are noise cancelling etc. A lot of this technology and knowledge was put into these cochlear implant technologies seen today and there are two or three companies doing this.
One of the biggest is an Australian company called Cochlear Corporation, who has made the technology very intelligent, so that a person can walk into a noisy restaurant and the processor can ignore or filter all of the background noise and focusing on the person who is talking to the implanted person. The quality of the sound the person is hearing now, is considered much more comfortable.
Initially, we started with adults and the brain has to learn again. Over time, as this technology became stable, we started implanting them in babies so that they could grow up hearing and speaking normally, because language is also linked to hearing. They found that the earlier you did the intervention, the better it was for the person, and today, these people can almost lead normal lives.
Vision restoration and Pixium's challenge is more complicated than the cochlear one but I'm very optimistic, if we could do it for the bionic hearing, we should be able to do it for bionic vision as well. It is a matter of learning and understanding the brain.
What level of the vision can you deliver currently? For example, is it possible for a parent to recognize a child's face?
This sort of question is difficult to answer, because ultimately, what is being asked is what does the person see? Vision and visual perception is very individual, I would love to be able to see inside the patient's visual cortex, deep in their brain to see what information is coming in and what are they seeing.
The only other tools we have in front of us is the words that people use to describe when we put objects and different shapes in front of them. For example, we have a patient who has a three-year-old and a seven-year-old and she described that as things got better, she could start seeing what kind of dresses they are wearing (dark or light) and that she can see the outline of their face if it is in a certain contrast with a background light. She can see somebody smiling or frowning, simple things that, with normal vision, are taken for granted.
Although she can describe something, it is not the same as visual face recognition. They describe it more as the outlines of a facial expression, but not the face at this point. We just don't have enough resolution yet in our technology.
We are dealing with millions of cells in the retina which are processing visual information and sending it to the brain. We're now trying to talk to them with 150 pixels, which is our current technology, and has to be intelligent enough to replicate bio-physiological work of millions of cells naturally over your lifetime, responsible for processing an image. We cannot say we are there yet in terms of face recognition, we are there in terms of outline of a person or an object at this point for some patients.
Why does treatment for blindness currently represent a major unmet medical need throughout the world?
The WHO estimate that 280-300 million people have vision impairment and around 40-45 million people are totally blind. That is similar to the size of a country like Spain. They have a deterioration in quality of life, suffer isolation, and dependency on others to do even basic tasks.
It is very different whether you're born blind, which is a very small percentage, roughly 4-5% of the blind population is congenital blind. Most of the blind population have acquired blindness and the main reasons for this is from cataract, glaucoma, diabetic retinopathy or age related macular degeneration, including retinitis pigmentosa.
Cataract is a treatable condition and blindness can be avoided. Glaucoma can be managed if treated early. Blindness from age related macular degeneration, particularly dry form, and retinitis pigmentosa have currently no curative solutions .
A blind person is statistically ten times more likely to have an accident and you see these people even with limited vision left, they're bumping into things, falling down stairs, etc.
Age related macular degeneration patients, even if they have some partial vision left, have a higher risk of depression. Most of these people who are progressively losing vision over time become more socially isolated. They have even been starting to get prescribed anti-depressants. This is a population that has a higher risk of premature death and earlier admission to nursing homes.
The costs of blindness to society and the macro dynamics aging populations, have a major social and economic burden to the society. There are many direct and indirect costs amounting to billions of dollars, to be considered.
These people are outside of the productive population and so they are unable to contribute, as well as being dependent on social aid. This accounts for billions of dollars or euros per year spent either on direct costs such as hospitalizations and treatments and prescriptions or drugs and anti-depressants etc., in addition to the indirect costs.
Costs as well as the qualitative aspect like quality of life impact, is what leads to a significant burden on society and the healthcare system.
What do you think the future holds for bionic vision restoration?
Pixium is today the only company which is working on addressing two diseases in parallel with two distinct retinal implant systems. The first one is the 150 electrode IRIS system designed to be exchangeble. This is an epi-retinal implant, it is the last decade's technology helping this rare disease called retinitis pigmentosa which affects 1 in 4,000 people.
With this rudimentary vision, which is useful or partial vision, our aim is to start getting it back. These are relatively young people, they, typically, by the age of 40s and early 50s have gone blind. Everybody works with this category of population because they have the greatest need. They are also the most demanding as well and they would like to get their vision back.
Then, you have the age related macular degeneration patients where the expectations are higher, but you also have more complexities. These are older population, so you cannot have a surgery which is very complex. For surgery today, general anesthesia for age related macular degeneration, you're looking at less invasive, ideally a local anesthesia surgery.
Pixium has developed the next generation system PRIMA, which is intended to improve the resolution from the current rudimentary outline of vision, shape, form, object, navigation, orientation, tool, life perception etc., aiming to start seeing or perceiving things in more detail. In order to do that, we have put it underneath the retina, really start stimulating directly from the layer of the photoreceptors i.e. rods and cones no longer functioning, and let the biology do part of the work this time.
You try to retrace the more biological pathway instead of starting at the last step at retinal ganglion cell level, before the signal enters the optic nerve. You start at the first layer, physically replacing the damaged photoreceptors by placing these totally wireless passive miniaturized micro-photodiodes at the same level. As there are no cables or wires, hence the one hour surgery, possible under local anaesthetic and place these little microchips, these little solar panels under the retina, at the back of the eye.
Light, emited from a pair of goggles with an integrated camera, is used to activate the implant. The signal passes more biologically through the bipolar cells this time, all the way to the ganglion cells before they enter the optic nerve and so the signal will be treated more biologically.
The promise, with all the research from the Stanford University, Vision Institute, the animal work and all the bench work we have done, tells us that signal should be richer in visual content than trying to do everything outside the body. This means that the further miniaturization of technology that has been achieved, in the next few months, we will have the first patients implanted with this next generation implant, the totally wireless subretinal PRIMA system.
Pixium Vision has pioneered this, partnering with the University of Stanford, and with Vision Institute in Paris, to start hopefully the first in human clinical study, which is planned to start later this year or early next year. That's the next milestone.
There are other reasons for blindness where other approaches are being considered, but that's a bit further down the road. In these scenarios, you're going to be involving neurosurgery at that point, because you are trying to directly tap into somebody's brain, and put a chip inside the brain. That's no longer ophthalmic retinal surgery at that point, but more invasive neurosurgery.
Pixium is not directly involved in that area, but we are continuously evaluating what will be the future. If you don't understand today, how the retina takes the information and pushes it all the way into the brain, going straight to the brain, it is a bit of trial and error approach and very invasive way of trying to recover something.
Pixium remains at the retinal level with two approaches, epi-retinal and sub-retinal. We want to understand better the less invasive pathway to the brain and try to understand what the brain is expecting.
Where can readers find more information?
About Khalid Ishaque
Mr. Khalid Ishaque has been the Chief Executive Officer of Pixium Vision SA since 2014. Mr. Ishaque spent 17 years with Boston Scientific Corporation, in various commercial and business development roles.
As General Manager of its Neuromodulation International business, he established and led the international sales and marketing operations for the fast growing division with Spinal Cord Stimulation for pain management and global market entry for Deep Brain Stimulation for movement disorders such as Parkinson's disease and dystonia.
Mr. Ishaque received postgraduate degrees in Engineering from Cranfield Institute of Technology in the UK and in International Economics and Management from SDA Bocconi in Italy.