As the world grapples with the COVID-19 pandemic, new questions arise as to the risk posed by the virus to different patient populations, including the elderly and those with underlying disease. A new study published on the preprint server medRxiv* in May 2020 deals with the risk of COVID-19 in the subgroup of patients with cancer.
Earlier studies showed a doubling of death rates in patients with cancer compared to the general population (5.6% vs. 2.3%). Cancer is among the coexisting conditions that increase the risk of severe COVID-19 disease. Chinese studies have shown that up to 54% of severe cases occurred in cancer patients with a higher rate of death, at up to 29%.
In contrast, more recent studies from China have shown that the mortality among cancer patients is closer to 5% to 10%, and is especially high among those with lung involvement, whether primary or secondary tumors. UK and US studies have contradicted these findings. The studies quoted here all rely on hospitalized patients rather than prospective cohorts of COVID-19 patients, which introduces bias into the outcome measures.
The current study was initiated at the Institut Curie following the national lockdown in France on March 6, 2020. The registry of cancer cases comes from the entire duration of the outbreak, as a result, and was designed to help answer questions about disease incidence, outcome among cancer patients, and risk factors for negative outcomes.
Population characteristics
There were about 9,800 patients in all, who attended the Institut Curie at least once. Of these, over 7,800 were on active treatment. The most common cancer by far was breast cancer, at 45%, followed by many other types at 5% to 6% each.
There were 141 patients registered in the cancer-COVID-19 registry, which gives an incidence of about 1.4%. The median age was 62 years, but a quarter was over 70. A fifth of the patients was obese. Over a third had high blood pressure, a fifth were smokers, and over 15% had diabetes.
Anticoagulants, ACE inhibitors, or ARBs for hypertension and corticosteroids were commonly used by a quarter, a fifth, and slightly below a fifth of patients. The type of cancer in this group followed the general trend but at a higher level, with breast cancer accounting for 40% followed by blood cancers and those of the female organs at 13%.
70% of patients with solid tumors had advanced cancer, and 41% had metastases in the lung. Only 39% were being treated with curative therapy for cancer.
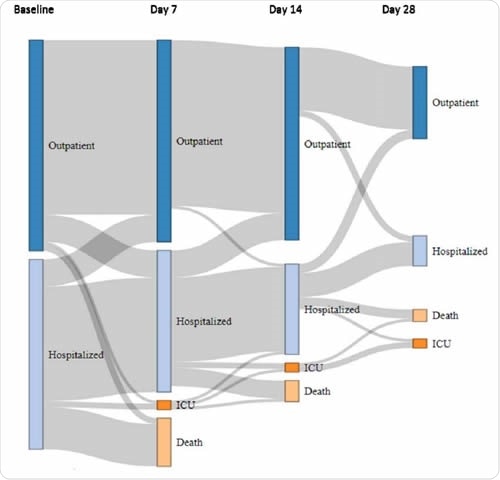
The patient trajectory from baseline to day 28. Diagram showing the changing status of cancer patients with COVID-19, based on individual follow-up. At baseline, patients were either immediately discharged home (dark blue bars) or hospitalized (light blue bars), including patients already hospitalized at the time of COVID-19 diagnosis (hospital-acquired infection). The patient's status may have changed on Days 7, 14, and 28 to one of the following four modalities: discharged home (dark blue bars), hospitalized (light blue bars), admitted to ICU (dark orange bars), and deceased (light orange bars). The grey flows between bars are proportional to the number of patients at each step
Patient evaluations revealed no significant differences in lung involvement in cancer patients with COVID-19. There were differences in the laboratory test results concerning the blood counts, but these had no clinical value.
Two-thirds of patients were discharged home, with only about 8% being transferred to the intensive care unit (ICU) at some point. Eventually, about a fifth of patients died of COVID-19, mostly those with lung cancer and blood malignancy. In total, 35 patients were transferred to the ICU or died, both of which were classified as a poor outcome.
The chief risk factors for a poor outcome included older age, male sex, the type of cancer (non-breast cancer and palliative therapy), and COVID-19 with lung symptoms and more extensive lung involvement. However, on multivariate analysis, only oxygen desaturation and evidence of lung damage on chest imaging were reliable predictors for death or ICU admission, increasing such odds by almost 7 and 2.5 times, respectively.
How did COVID-19 affect cancer care?
In almost 70% of cases, the doctors stopped chemotherapy, targeted therapy, and current radiation therapy. Immune checkpoint inhibitor therapy was stopped in over 80% of patients. Elective surgeries were postponed in almost 80% of cases for three weeks on average.
Why is this study important?
This study is the first prospective study of cancer patients with COVID-19, including both hospitalized and outpatient populations. The results fall into three groups:
An incidence rate of 1.4% among cancer patients overall, or 1.7% when only those with active disease are considered. This is possibly an underestimate but falls within the 5.7% estimate for France as a whole.
When compared with the 12.3% incidence of infection in the area where the Institut Curie is located, this indicates that as a whole, cancer patients are not a higher risk for COVID-19 compared to the general population when under lockdown conditions.
The clinical features of COVID-19 in such patients are also comparable to those in the general population. The mortality in both groups is about 20% and was predicted by characteristics of COVID-19 rather than cancer unless the latter was recently diagnosed.
Cancer inpatients with COVID-19 had the same risk of death. Some reasons for this could be the use of anticoagulants, which possibly prevented thromboembolism. Immune exhaustion or pre-existing inflammation could explain the failure to observe a cytokine storm in this population.
Impact of COVID-19 on cancer care
In almost two-thirds of cases, cancer treatments could not proceed as scheduled. Another study by the same researchers shows a drop in primary consultations for breast cancer by over a third, compared to the same period of time in 2019. This could have a pronounced effect on cancer while also putting a strain on cancer-related health resources.
Breast cancer patients may be overrepresented in this study, which could have led to a false improvement in the outcome statistics. However, the patient configuration is similar to that of other centers that offer comprehensive cancer care.
The researchers conclude, “Our findings strongly suggest that COVID-19 is neither more frequent nor more fatal in cancer patients as a whole. A simple baseline clinical assessment combining O2 saturation measure and a chest CT scan clearly identifies patients at risk of poor outcome and should be widely recommended in cancer patients with suspected COVID-19.”
This study, combined with better epidemiologic data based on broad-based antibody testing and more extended periods of follow up, should help to evolve better care for cancer patients while the pandemic is going on.

 This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
This news article was a review of a preliminary scientific report that had not undergone peer-review at the time of publication. Since its initial publication, the scientific report has now been peer reviewed and accepted for publication in a Scientific Journal. Links to the preliminary and peer-reviewed reports are available in the Sources section at the bottom of this article. View Sources
Journal references:
- Preliminary scientific report.
Basse, C., et al. (2020). Characteristics and Outcome Of SARS-Cov-2 Infection in Cancer Patients. medRxiv preprint. doi: https://doi.org/10.1101/2020.05.14.20101576. http://medrxiv.org/cgi/content/short/2020.05.14.20101576
- Peer reviewed and published scientific report.
Basse, Clémence, Sarah Diakite, Vincent Servois, Maxime Frelaut, Aurélien Noret, Audrey Bellesoeur, Pauline Moreau, et al. 2021. “Characteristics and Outcome of SARS-CoV-2 Infection in Cancer Patients.” JNCI Cancer Spectrum 5 (1). https://doi.org/10.1093/jncics/pkaa090. https://academic.oup.com/jncics/article/5/1/pkaa090/5920243.