The coronavirus pandemic is actively spreading across the globe, with millions of people infected. Amid the global health crisis, scientists race to develop an effective vaccine against the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection.
Many vaccine candidates against the novel coronavirus target the viral spike protein, but there is limited information on the quality of antibody responses generated with these vaccines. Now, a team of scientists from the Center for Biologics Evaluation and Research at the U.S. Food and Drug Administration (FDA) aimed to evaluate vaccine-induced antibody responses in an animal model.
Spike protein target
To successfully initiate infection, viruses need to surpass the cell membrane barrier. Viruses that are enveloped attain this via membrane fusion, a process that is mediated by specialized fusion proteins.
Though the SARS-CoV-2 uses various proteins to replicate and infect cells, the spike protein is the key surface protein that it utilizes to bind to a receptor, the angiotensin-converting enzyme 2 (ACE2). The ACE2 acts like a doorway into the cell.
After the spike protein binds to the receptor, the membrane of the virus fuses with the human cell membrane, allowing the virus genome to enter human cells and trigger an infection. Most vaccine candidates aim to prevent the attachment and fusion of the spike protein to avert infection.
Multiple versions of the SARS-CoV-2 spike protein are currently being evaluated as vaccine candidates using a multitude of modalities and delivery systems. At present, there is limited data for the immune responses produced after vaccination by the spike protein vaccine candidates.
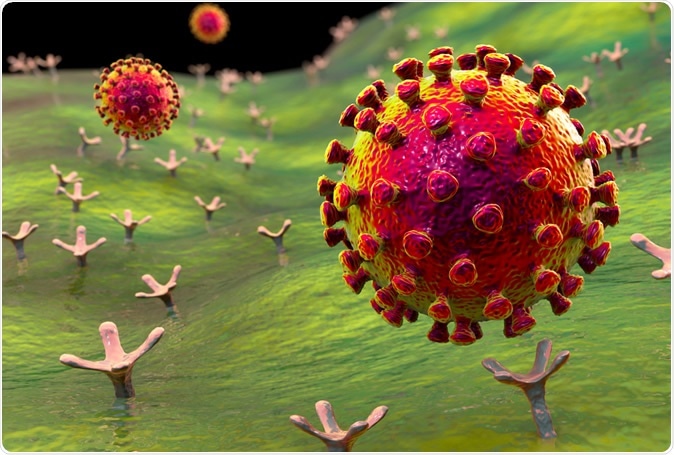
SARS-CoV-2 viruses binding to ACE-2 receptors on a human cell, the initial stage of COVID-19 infection, conceptual 3D illustration credit: Kateryna Kon / Shutterstock
Unique immune responses
The team wanted to provide an insight on the humoral immune response produced by different vaccine antigens, such as functional activity, antibody epitope repertoire, and antibody binding activity. To arrive at their findings, the research team vaccinated rabbits with various spike proteins of SARS-CoV-2, including the S1+S2 or spike ectodomain, the S1 domain, the S2 domain, and the receptor-binding domain (RBD). These spike proteins were either produced in mammalian cells or insect cells.
The scientists conducted an in-depth evaluation of the antibody response triggered by various SARS-CoV-2 spike antigens that are akin to the vaccine antigens used in clinical development.
They found that the serum generated by the various spike proteins, such as S1+S2 ectodomain, RBD, and the S1 domain, was able to neutralize the virus by 50 to 60 percent in SARS-CoV-2-FBLuc single-cycle pseudovirus neutralization assay in Vero E6 cells after a single dose of the vaccine. After two doses of the vaccine, there was the neutralization of 93 to 98 percent.
Further, the team noted that the RBD-immune serum appeared to have better functional activity than the other vaccine antigens due to a higher affinity antibodies post-vaccination of the second dose. Meanwhile, the team discovered that the S2 domain did not generate as many neutralizing antibodies, unlike the S1 domain and RBD. Based on the enzyme-linked immunosorbent assay (ELISA), the S2 domain contains the fusion peptide but did not seem to be as immunogenic in producing binding antibodies.
The scientists concluded that RBD immunization might be the most effective since it was able to generate more high-affinity antibodies than the other vaccine types. In studies about other viral infections, high-affinity antibody responses were tied with clinical benefit in infected individuals. Vaccines that produce high-affinity antibodies may improve the clinical outcome of SARS-CoV-2 infection.
“Therefore, in addition to measurements of antibody binding titers and virus neutralization, this and the previous studies demonstrate the importance of assessments of antibody affinity maturation during SARS-CoV-2 vaccine trials,” the team concluded.
“In addition to designing the best immunogen, selection of appropriate adjuvant could drive responding B cells into affinity maturation in germinal centers, as previously observed in clinical trials of influenza vaccines,” they added.
The study underlines the need to conduct a comprehensive analysis of the immune response generated after vaccination or SARS-CoV-2 infection. This may help determine the biomarkers of protective immunity. A better understanding of the immune responses produced by different spike protein vaccine antigens can help in the development of effective drugs and vaccines against the coronavirus disease.
A dire need for a vaccine
As scientists across the globe race to find an effective vaccine against the SARS-CoV-2 infection, the world grapples with skyrocketing infections and deaths. So far, the coronavirus disease (COVID-19) has taken the lives of more than 416,000 people and infected roughly 7.35 million worldwide.
The United States reports the highest number of confirmed cases, nearly 2 million infections. The country’s death toll has topped 112,000. Meanwhile, Brazil, Russia, and the United Kingdom follow with 772,416 cases, 493,023 cases, and 291,588, respectively.
Source:
Journal reference: