Studies have shown that severe coronavirus disease 2019 (COVID-19) correlates with lymphopenia and low T cell concentrations, and mild COVID-19 correlates with a strong T cell response to severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection. While most individuals infected with SARS-CoV-2 produce neutralizing antibodies, the effectiveness of this antibody response may be partly compromised by the loss of CD4 T follicular helper cells and increased extrafollicular B cell expansion seen in severe COVID-19.
The immune response to SARS-CoV-2 also includes innate immune cytokine release, including IL6, IL8, and 26 CXCL10/IP10. IP-10 shows strong correlation with severe clinical outcomes and CXCR3 has been shown to be involved in the trafficking of antiviral T cells to tissue compartments.
How does HIV infection affect COVID-19 disease?
Not much is known about how HIV modulates the immune response to COVID-19. HIV can cause dysregulation of T cell responses, which in turn can cause B cell dysregulation and dysfunction. Thus, HIV co-infection will likely change the COVID-19 immune response.
Epidemiological studies have obtained mixed results on the interaction of HIV and SARS-CoV-2. Many extensive studies have observed that HIV co-infection can increase mortality risk in COVID-19 by approximately 1.5 to 3-fold, while most of these studies found no statistically significant changes in clinical presentation.
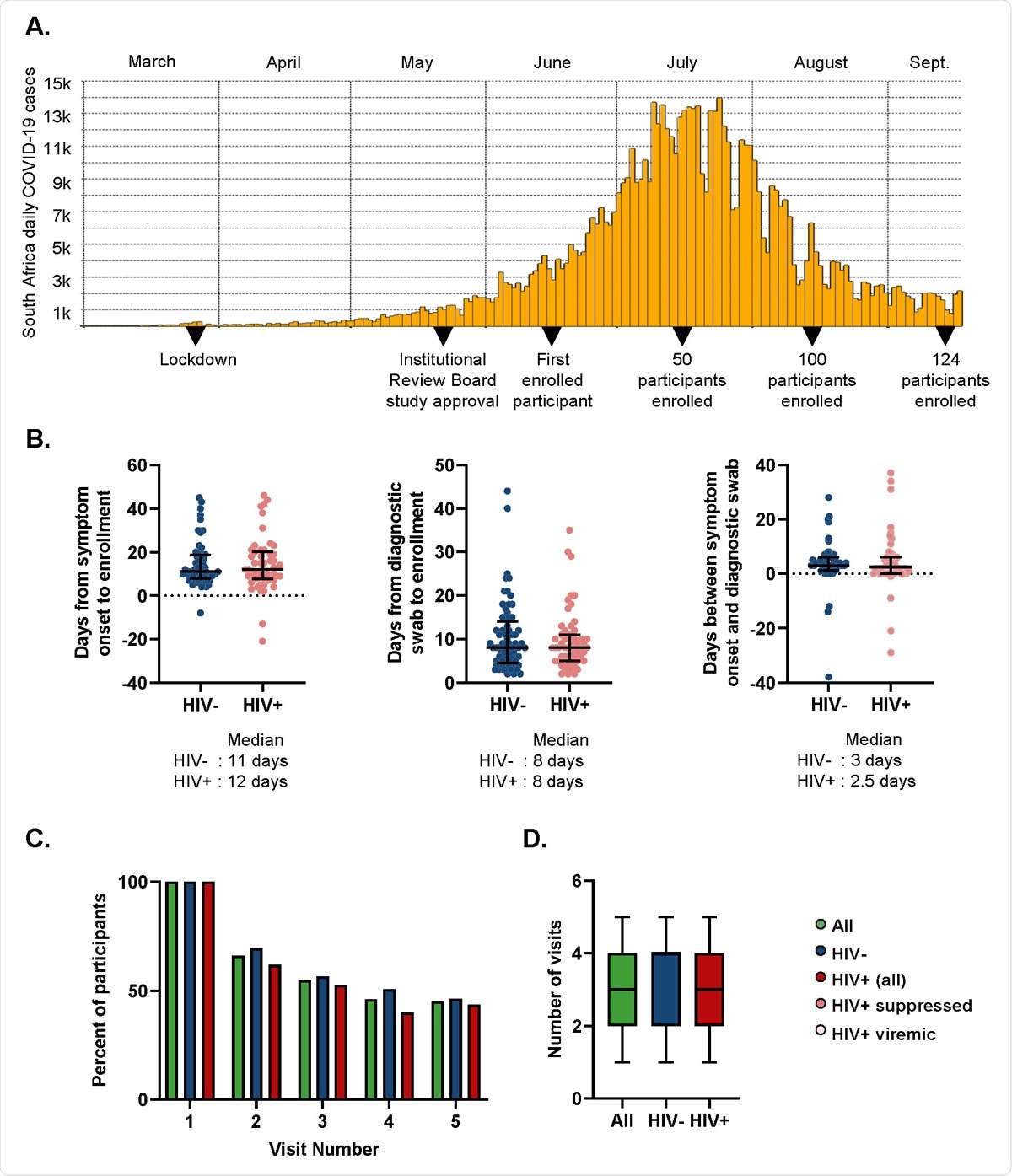
Study characteristics. (A) Study timeline. (B) Time from symptom onset or diagnostic swab to study enrollment for symptomatic participants. Left panel shows time elapsed for HIV negative (blue points) and PLWH (red points) between symptom onset and enrollment. Middle panel shows days from the time the diagnostic swab was taken to enrollment for HIV negative and PLWH. Right panel shows time difference between symptom onset and diagnostic swab. (C) Percentage of participants attending follow-up visits for all participants (green), HIV negative (blue), and PLWH (red). (D) Number of visits (from a total of 5 study time-points per participant) for each participants. Median and IQR for all participants (green), HIV negative (blue), and PLWH (red).

 *Important notice: medRxiv publishes preliminary scientific reports that are not peer-reviewed and, therefore, should not be regarded as conclusive, guide clinical practice/health-related behavior, or treated as established information.
*Important notice: medRxiv publishes preliminary scientific reports that are not peer-reviewed and, therefore, should not be regarded as conclusive, guide clinical practice/health-related behavior, or treated as established information.
Impact of HIV on COVID-19 immune response in an African region with high HIV prevalence
In a preprint paper published on the medRxiv* server, a team of researchers from various institutions in South Africa, the UK, and Europe discuss how they determined the impact of HIV on the COVID-19 immune response in KwaZulu-Natal, South Africa, which is an area with very high HIV prevalence. The researchers believe that this study will help understand the long-term consequences of COVID-19 infection and the vaccination response in this population.
The team investigated used four longitudinal samples from 124 study participants from KwaZulu-Natal, South Africa. 44% of the participants were people living with HIV and had other co-morbidities such as hypertension, obesity, and diabetes.
COVID-19 immune response differed significantly between people living with HIV and HIV negative participants
Most people living with HIV showed CD8 T cell expansion above the normal range after a SARS-CoV-2 infection. In participants who underwent antiretroviral therapy to suppress HIV, CD8 expansion was associated with milder COVID-19 disease.
There were many differences in T cell, B cell, and natural killer cell correlations in people living with HIV and participants who were HIV negative. Lower tissue homing CXCR3+ CD8 T cells in the presence of SARS-CoV-2 RNA was seen in people living with HIV, but not in HIV negative participants. There was a pronounced early antibody-secreting cell expansion in HIV-negative individuals, while this was absent in people living with HIV.
Low CXCR3 correlated with increased COVID-19 severity across groups, while high antibody-secreting cells correlated with increased disease severity in HIV negative individuals and waned once SARS-CoV-2 was cleared.
HIV infection status did not affect the severity of COVID-19 disease
Overall, the results show that despite the altered immune response, COVID-19 disease was mostly mild in people living with HIV, similar to participants who were HIV negative. This is likely a reflection of the heterogeneity of an effective COVID-19 immune response. It is yet to be determined if the differences in immune responses in people living with HIV will compromise vaccination or lead to different long-term consequences.
“We have shown that HIV infection changed the immune cell response but not clinical outcomes or symptoms of COVID-19 infection.”
The researchers also observed that HIV viremia affects the COVID-19 immune response in people living with HIV, including consistently elevated CD8 T cell levels whether or not SARS-CoV-2 RNA is present and the lack of CD4 T cell recovery after SARS-CoV-2 clearance. Hence, effective ART suppression likely has a role in attenuating the effects of HIV infection on the immune response to COVID-19.
“Given that COVID-19 infection outcomes were similar in PLWH relative to HIV negative participants, the differences in immune response between the groups may indicate an alternative, as opposed to dysregulated, immunity to SARS-CoV-2 in PLWH.”

 *Important notice: medRxiv publishes preliminary scientific reports that are not peer-reviewed and, therefore, should not be regarded as conclusive, guide clinical practice/health-related behavior, or treated as established information.
*Important notice: medRxiv publishes preliminary scientific reports that are not peer-reviewed and, therefore, should not be regarded as conclusive, guide clinical practice/health-related behavior, or treated as established information.