Too much of a good thing? A new study reveals that while healthier gut-friendly diets lower infertility risk, going beyond a certain dietary threshold may reverse the benefit, underscoring the need for balance in nutritional planning.
 Study: Association between the dietary index for gut microbiota and female infertility: a cross-sectional study of NHANES 2013–2018. Image Credit: New Africa / Shutterstock
Study: Association between the dietary index for gut microbiota and female infertility: a cross-sectional study of NHANES 2013–2018. Image Credit: New Africa / Shutterstock
In a recent study in the journal Frontiers in Nutrition, researchers investigated the association between the novel Dietary Index for Gut Microbiota (DI-GM) and female infertility. The study aims to inform future dietary interventions against the condition. It used questionnaire-based approaches to evaluate 3,053 adult women (age = 18–45), 12.12% of whom were revealed to be infertile.
Study findings demonstrated a complex non-linear association between DI-GM scores and infertility. While lower scores generally correlated with higher infertility risk, the analysis revealed an inflection point: above a certain DI-GM score (specifically, a score of 8), the risk of infertility paradoxically increased. These findings suggest that future gut microbiota research and dietary interventions may help address infertility’s silent pandemic, emphasizing the need for a balanced approach rather than simply maximizing DI-GM.
Background
Infertility, the medical condition characterized by an individual’s inability to achieve a clinical pregnancy even following 12 months of frequent unprotected sex, is a growing global public health concern. Current estimates report that 12.5% of all couples of childbearing age suffer from the condition, with genetic, lifestyle, and environmental factors implicated in its incidence. Alarmingly, several health agencies classify infertility as the third most important threat to public health, following cardiovascular diseases (CVDs) and cancers.
“Common etiologies include ovulatory dysfunction, endometriosis, polycystic ovary syndrome (PCOS), fallopian tube abnormalities, and immunological disorders.”
Recent research on female infertility has highlighted diet as a potentially modifiable healthy behavior with modulatory impacts. Parallel studies on the gut microbiome suggest a link between gut health and female reproductive diseases. The strong influence of dietary patterns over gut microbiota composition and performance suggests dietary interventions as a non-pharmaceutical weapon in clinicians’ arsenals against infertility.
While studies have explored links between general diet/gut microbiota and female reproductive health, the specific relationship between the DI-GM index and female infertility remained unexplored prior to this study.
About the study
The present cross-sectional study investigates the association between DI-GM, a newly introduced gut microbiota index developed by Kase et al., and female infertility. Study data were obtained from the National Health and Nutrition Examination Survey (NHANES) database (2013–2018) and focused on non-pregnant adult American females (age = 18–45).
Kase et al.’s scoring system was used to compute GI-GM scores using all 14 of the index’s food and nutritional components. Participant data were obtained via 24-hour dietary recall questionnaires with DI-GM scores ranging from 0 to 13.
“The DI-GM includes 10 beneficial components (avocado, broccoli, chickpeas, coffee, cranberries, fermented dairy, fiber, green tea, soy, and whole grains) and four unfavorable components (red meat, processed meat, refined grains, and high-fat diets). We averaged the results from two 24-h dietary recall interviews for each participant to calculate the DI-GM scores.”
Female infertility was assessed using questions (n = 2) from the Reproductive Health Questionnaire (RHQ074 and RHQ076). Additional participant data included demographic, lifestyle, health, and reproductive health details alongside records on infections and inflammatory disease. Statistical analyses leveraged weighted linear regression models, chi-square tests, and weighted multivariate logistic regression models.
Study findings
Of the 29,400 NHANES participants, 14,452 were excluded for being male, 10,625 were excluded for being outside the inclusion age, and 614 were excluded for incomplete information, leaving a final study dataset of 3,053 eligible individuals. Of these, 370 (12.12%) were revealed to be infertile, with infertile participants found to be, on average, older, having a higher body mass index (BMI), married, current smokers, and were more likely to suffer from (or be under treatment for) pelvic diseases or metabolic conditions.
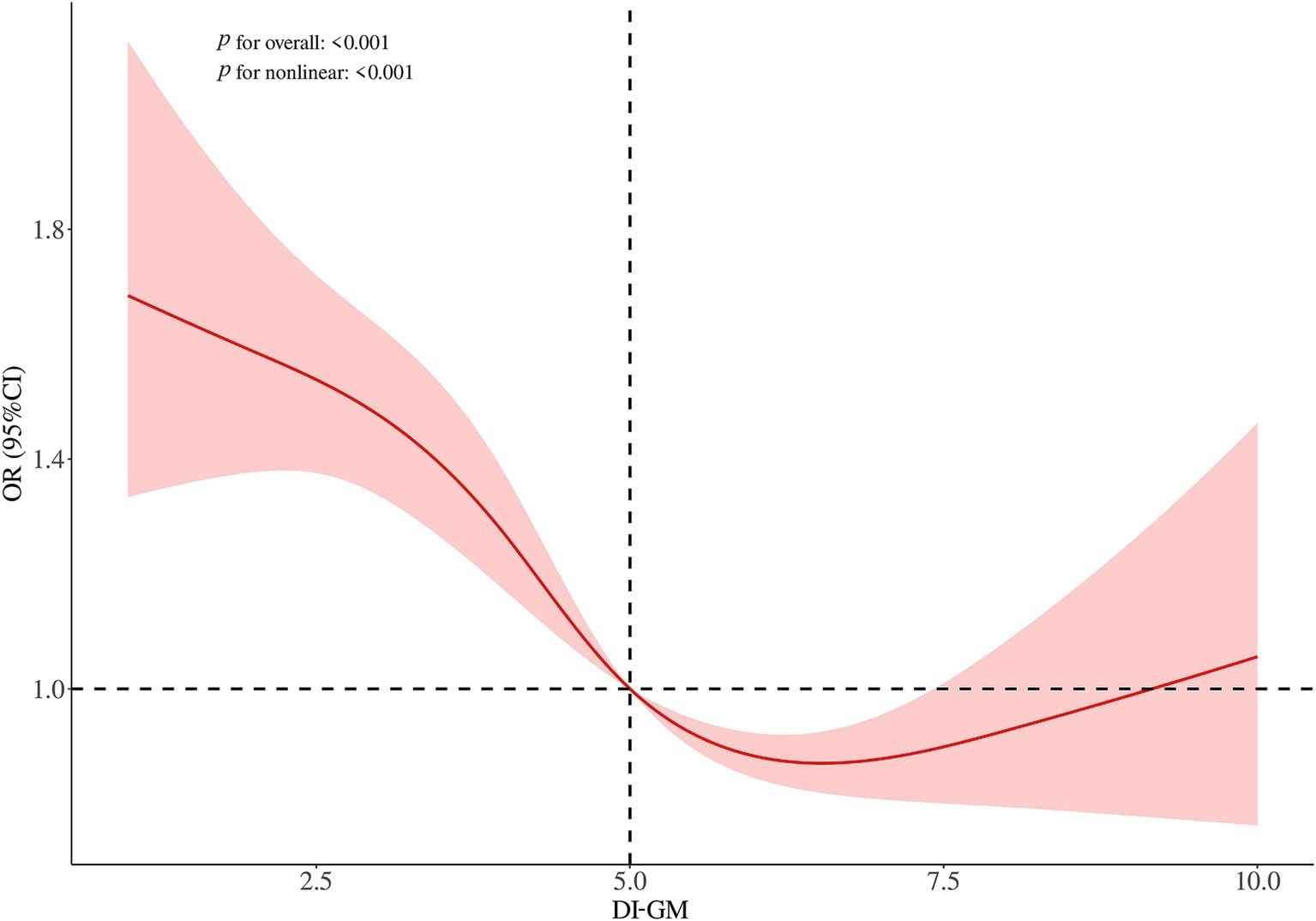 Restricted cubic spline plots for the association between DI-GM and infertility in women. Adjusted for age, ethnicity, education level, PIR, marital status, smoking, drinking, dyslipidemia, diabetes, hypertension, menstrual status, PID, birth control pill use, and female hormone use.
Restricted cubic spline plots for the association between DI-GM and infertility in women. Adjusted for age, ethnicity, education level, PIR, marital status, smoking, drinking, dyslipidemia, diabetes, hypertension, menstrual status, PID, birth control pill use, and female hormone use.
DI-GM investigations revealed that infertile participants demonstrated significantly lower DI-GM scores than their fertile counterparts on average. Logistic regression analyses initially suggested a negative association between DI-GM scores and infertility outcomes when treated as a continuous variable or in quartiles. However, RCS analysis further revealed this association to be non-linear. Crucially, a threshold effect analysis identified an inflection point at a DI-GM score of 8. Below this threshold, higher DI-GM scores were associated with a reduced risk of infertility. Conversely, for scores above 8, higher DI-GM scores were unexpectedly associated with an increased risk of infertility.
“Participants with lower DI-GM scores also exhibited higher triglyceride levels and fasting plasma glucose (FPG) and lower high-density lipoprotein cholesterol (HDL-C) levels (p < 0.05). Additionally, the prevalence of infertility among participants significantly decreased from Q1 to Q4 (p = 0.041), with notably lower rates observed in Q3 and Q4 (11.18 and 11.17%, respectively) than in Q1 and Q2 (16.32 and 16.16%, respectively). These observed variations suggest that the potential association between DI-GM and infertility requires further investigation.”
Subgroup analysis did not alter these findings, with observed relationships remaining robust demonstrated across a spectrum of subgroups.
Conclusions
The present study demonstrates a complex, non-linear relationship between gut microbiota indices (herein DI-GM) and female infertility. While higher DI-GM scores up to a certain point appear protective, very high scores (above 8) were linked to increased risk. This highlights the potential for dietary interventions and future gut microbiota interventions against the rising global concern, emphasizing that achieving a balanced dietary pattern reflected by an optimal DI-GM range, rather than simply maximizing the score, may be key.
“As a new dietary quality index that reflects gut microbiota diversity, further research and interventions using DI-GM could help develop strategies to prevent and reduce the risk of female infertility.”
Journal reference:
- Zhang, X., Wu, L., Li, H., Zhang, S., & Hua, W. (2025). Association between the dietary index for gut microbiota and female infertility: a cross-sectional study of NHANES 2013–2018. In Frontiers in Nutrition (Vol. 12). Frontiers Media SA, DOI – 10.3389/fnut.2025.1583805, https://www.frontiersin.org/journals/nutrition/articles/10.3389/fnut.2025.1583805/full